Dating with Chronic Illness (and What I’ve Learned)
Dating with Chronic Illness – A Thorny Topic Dating with chronic illness is no easy, straightforward feat for either party. Questions like this are all over Quora and Reddit: “Would you date or marry a person with chronic illness?”. So I thought I’d share my […]
Chronic voicesEasy Gluten-Free Finger Foods Everyone Will Love
Are you looking for gluten-free finger foods for your next party that everyone will enjoy? We have you covered! Preparing gluten-free party bites doesn’t have to be complicated. Whether you’re hosting a Superbowl party, game night, baby shower, bridal shower, or holiday gathering, this collection […]
mind-&-emotions
My Personal Experiences with Epiphrenic Esophageal Diverticulum (Plus Tips to Help Cope)
Two New Diagnoses – Epiphrenic Esophageal Diverticulum & Mitral Valve Stenosis Whilst I haven’t heard much good news in a long time, I did not expect 2025 to be a harbinger of such terrible news. It seems like I will need to get two major […]
Chronic voices
Dating with Chronic Illness (and What I’ve Learned)
Dating with Chronic Illness – A Thorny Topic Dating with chronic illness is no easy, straightforward feat for either party. Questions like this are all over Quora and Reddit: “Would you date or marry a person with chronic illness?”. So I thought I’d share my […]
Chronic voicesDating with Chronic Illness – A Thorny Topic
Dating with chronic illness is no easy, straightforward feat for either party. Questions like this are all over Quora and Reddit: “Would you date or marry a person with chronic illness?”. So I thought I’d share my perspective, as a person who’s chronically ill and disabled. Over the years, I’ve been in long-term, short-term and even long-distance relationships. I’ve also tried various dating apps, and met partners through friends. I much prefer the latter, but it does get harder the older you get!
P.s. The original version of this post was published on 26 February, 2017 (8 years ago!). More insights into dating, relationships, self-worth, disability and chronic illness have been added 🙂
*Disclaimer: This article is meant for educational purposes, and is based on my personal experiences as a patient. Whilst I have done my utmost to be meticulous in research, I am not a doctor, and nothing in this article should be substituted for medical advice. Please consult your own doctor before changing or adding any new treatment protocols. This post may also contain affiliate links. It will cost you nothing to click on them. I will get a small referral fee from purchases you make, which helps with the maintenance of this blog. Read our Privacy Policy page for more information. Thank you!
Pin to Your Dating & Chronic Illness Boards:
Just Like Chronic Illness, Every Relationship is Unique
I’ve been fortunate enough to have had relationships with partners from extreme ends of the spectrum. It gives me insight into different perspectives, which enables me to identify and appreciate certain characteristics better. Their opinions about our future together were diverse, and so were their attitudes towards my daily health struggles. Before going further, I’d like to state that the purpose of this article isn’t to bash anyone at all. Everyone is entitled to how they want to live their lives, and who they want to do that with, for better or for worse.
Partners Who Saw My Chronic Illnesses as a Liability
My first relationship was with a guy whose greatest desire was to start a family of his own, and it troubled him that I never seemed to get better. He did not like the open-ended, variable timetable of my chronic illnesses. Neither did he want to start with a ‘deficit’ before even trying for a child.
I underwent a few surgeries whilst we were dating, and he felt tormented that he could do ‘nothing’ to make it better. Yet, he never provided any emotional support, and would often bail out on the bad days. I ended up having to be stronger for him, because ‘it was difficult for him too’. I would always give in to him, because I thought that I had less rights to my own opinions. It was already a burden for someone to be with me, what more could I ask for?
Dates Who Tried, Then Ran
I’ve also dated men who were willing to try things out for a couple dates, but who were constantly analysing my limits. This isn’t too fair in my opinion for several reasons. First, I have good and bad days, and you might be seeing me during a bad week. Second, and this is applicable to healthy individuals, too – it takes a bit of time to truly know who a person is, both the good and bad. Third, their assessment of my capabilities is usually inaccurate, because it tends to be biased. Unfortunately, when you’re chronically ill or disabled, people tend to hyperfocus on the limitations and judge you more keenly and immediately.
Then there are those dates where they see me arrive with a walking stick on a bad day. We have a short, polite chat, before they run for the hills and hide themselves behind a wall of silence. Whilst this feels unpleasant, I have learned to accept that it’s all part of the dating game, sick or otherwise.
Divorced Partners are Not Necessarily More “Chill”
There was a period of time I said to myself, “well, let’s wait for all the married men to get divorced. They should be wiser and more open-minded now, and realise that there’s more to a relationship than chronic illness”.
This turned out to be false. I obviously can’t speak for all divorced men, but the ones I have personally interacted with were fairly extreme. They were either paranoid (“you haven’t replied to my message in 24 hours, even though there are two blue ticks!”), or fixated on a certain ideal (hyperfocused on a singular quality, to the exclusion of all other qualities). Chronic illnesses still bothered most of them. Divorced men are not necessarily wiser than an unmarried person. They are still human, with strengths and flaws alike.
-
Read Related Posts:
- Disability & Sex: Disabled People are Not Automatically Bad Sexual or Romantic Partners
- Chronic Illness is Unpredictable, but You Don’t Always Have to Fear the Unknown
- Life with Chronic Illness: Happiness & Pain Can Co-exist
- Today is Not a Good Day to Make Decisions (and That’s Okay)
- The Stories We Tell Ourselves: Prisons or Paths to Freedom
Partners Who Were Accepting of My Chronic Illnesses
My next partner always saw the future in a hopeful light, and went with the flow of life. For example, he believes that healthcare and medicine can only improve as more scientific advances are being made. He saw me at my worst, yet never once treated me as a lesser human being.
I know for sure that life will never be easy with me, yet it was a non-issue to him. He claims that there is nothing wrong with me at all, and that I didn’t affect his lifestyle. Another revelatory phrase he made was that every relationship has its own set of problems anyway, whether the partners were sick or healthy. (You can read more brilliant utterances about relationships he made in this post.)
I found that I grew with him as a person, because of his support to the very end. He never undermined any desire I had for education, which comes in many forms. Apart from the intellect, it also consists of life skills, hobbies, and most importantly, self-awareness.
Mental and invisible health issues are often seen as suspicious in the eyes of the public, but I never felt stigmatised by him. I could display my psychological and physical pains at the level of torture that they were truly at. That brought so much relief – just to have someone who believes you, and who never belittles the impact your experiences have on you.
Whilst we have broken up, we are still friends, and I visit him and his family every Christmas. I am genuinely happy for him, because I believe people like him truly deserve the best that life has to offer.
-
Read Related Posts:
- What’s it Like to be a Caregiver for a Chronically Ill Loved One (The Challenges & Rewards)
- Why Self-Acceptance is Important When You Have a Chronic Illness
- 365 Mindfulness Journaling Prompts for Self-Improvement
- Fun Things To Do While Recovering From Surgery: Hobbies, Crafts & Games (Part 3/5)
- What’s It Like Going Back to School as an Adult with Disability and Chronic Illness
The Most Important Thing I’ve Learned from Dating with Chronic Illness
If there’s one I’ve learned over the years from dating as a person with chronic illness, it is to have some respect for myself. If I were dating someone who treated me with contempt, resentment or blame, then I – a person with chronic illness and disability – would leave them.
With age, experience and the freedom I have had to grow, I’ve learned that I am worth just as much as any other person out there. So what if my illnesses are permanent? There is only one me amongst the billions of us on this planet, and we are all worth something in that regard.
In fact, an aura of quiet self-confidence and knowing your inherent self-worth can be attractive traits to potential partners. You are as deserving of love as any other human being; we are all part of the same world, and return to dust just the same.
“I’ve learned that I am worth just as much as any other person out there..There is only one me amongst the billions of us on this planet, and we are all worth something in that regard.” #SelfWorth #ChronicIllness #disability #relationships
Share on X
All Human Beings Need a Little Help to Get by in Life
There is no doubt that a person with chronic illness will need more help than someone who is healthy just to get by. Many situations might test your patience, question your love and flirt with your morality. In modern day culture, independence is a revered trait, and we like to think that we are independent beings.
But that is not how humanity has thrived over the centuries. We are social creatures built for community. It is an important aspect of social well-being. Yes, even introverts need a touch of human connection every now and then, in order to thrive.
And no human being is truly independent, anyway; just cut off their oxygen supply for a minute. We all depend on something to survive and thrive – a relationship with a chronically ill or disabled person also has the potential to help you develop as a person, and to live a fulfilling life ultimately. Perhaps even more so, because it will force you to reflect on your priorities, purpose and goals in life more than you would otherwise.
Pin to Your Dating & Life Lessons Boards:
-
Read Related Posts:
- Are You a Capable Person? What Does That Even Mean?
- I Have No Purpose in Life, and Therein Lies My Life Purpose
- Call Me Sick Girl (Or How to Make Your Weakness Your Strength)
- Asking for Help (and Why Everyone Needs to Learn this Important Life Skill)
- How to Use the 7 Dimensions of Wellness to Thrive with Chronic Pain
How Chronic Illness & Disability has Influenced the Way I Approach Romantic Relationships
To be honest, after having faced several life-and-death situations, I’ve become more stoical than I already was to begin with. Acceptance took me years to grasp, and I often need to learn to accept a new diagnosis all over again. However, I will vouch that it is the best coping tool and strategy that has enabled me to live my life, despite chronic illness. And if we’re being completely honest here, I am still grieving the loss of function in my knees. Grief and acceptance are two sides of the same coin; they come and go like visitors, and are not linear processes.
I actually adopt this mindset of acceptance when I approach relationships and dating with chronic illness as well. “Whatever will be, will be”, “que Será, Será”. For example, I never worry if my partner is going to cheat on me. If they do, then I will just up and leave – obviously it wasn’t meant to be.
Interestingly, this bothered a boyfriend, as he assumed that it meant that I didn’t like him enough to care. However, I’ve dealt with way more harrowing experiences, so I consider many everyday problems as trivial. You could say that it’s a bit like scar tissue – tougher, but less sensitive, which can be both a good and bad thing.
Pin to Your Chronic Illness, Disability & Relationships Boards:

-
Read Related Posts:
- An Experience from Hell: Pulmonary Embolism, DVTs & Antiphospholipid Syndrome
- What It Feels Like to be Suddenly Disabled
- What it Feels Like to be Refused Treatment by a Hospital’s A&E / ER
- My Personal Experiences with Epiphrenic Esophageal Diverticulum (Plus Tips to Help Cope)
- Interview on ‘The Uninvisible Pod’: What I’ve Learned From Living with Chronic Illness for 20 Years
Other Insights I’ve Gained from Dating with Chronic Illness & Disability
Whilst it is true that anyone can become disabled at any time, this fact doesn’t sink into healthy people’s brains regardless. I can’t blame them for that, as the devastation of chronic illness and disability is impossible to grasp, unless you live that reality yourself. Humans are also wired for self-preservation. This means that they instinctively avoid things that may contribute towards the eradication of their lives or legacies.
If I’m going to be logical, health is wealth. Who doesn’t want to be healthy? So yes, we are starting out with a deficit in life. However there is an extremely fine line between worth1 and worth2 that people often confuse. What do I mean by that? This statement from Positive Psychology helps to clarify it a little:
“Self-esteem is what we think and feel and believe about ourselves. Self-worth is recognizing ‘I am greater than all of those things.’ It is a deep knowing that I am of value, that I am loveable, necessary to this life, and of incomprehensible worth.”
In brief, people often confuse self-worth – where every human being is inherently valuable, and deserving of love and respect – with material or tangible value. It’s an issue of feeling secure or insecure. In a ‘modern’, capitalist era, it’s not that much of a shocker either, as we’ve been exposed to such ideals from our childhoods, and our parents may have even placed an emphasis on it.
Pin to Your Dating with Chronic Illness & Disability Boards:

My Best Tips for Dating with Chronic Illness
The communication style, character, values, sense of humour and lifestyle of all the people I’ve dated were vastly different. So it’s been an interesting, though admittedly exhausting, ride thus far.
I also broke both my knees fairly recently, no thanks to Lupus and long-term steroid treatment, plus developed yet more chronic diseases. These unasked for additions have definitely made dating much harder, as my disabilities become more and more apparent. Sure, rejection from being chronically ill and disabled stings, but it’s also for the best. I would be walking on eggshells, if I were with a partner whom I had to constantly prove and pretend I was healthy to.
Dating Tips for the Chronically Ill & Disabled
Here are a few of my personal golden rules, when it comes to dating with chronic illness and disability. Your list might look different, based on your own comorbidities, life experiences and personality.
- Have some self-respect. If a potential partner disrespects you in any way, leave. It’s better to be single than with someone who doesn’t treat you right. This will only compound problems in your life, such as mental health issues.
-
Be open-minded and explore. Yes it’s true – the more nets you cast, the more fish you get. This strategy definitely doesn’t work for everyone, due to a myriad of reasons, such as limited energy, religious beliefs, etc. But I believe in trying things out.
I mean, it’s just one date over coffee or dinner. At worst, you waste some time and discover that you’re incompatible. The reasons may not even be related to chronic illness – it happens to regular people, too. At best, you find your special person. Whilst I’m not an extrovert, I take it as an opportunity to socialise. I also believe that I can learn something from every person I meet – even from the bad dates. In that sense, there is no loss.
- Do they offer to pay for the first date? I am definitely not looking for a free meal and will refuse the offer, but this simple act of generosity tells me a few things. Basically, if they can’t even be generous financially, which is arguably the easiest, then how generous can they be with other more important or ‘difficult’ aspects of life, such as quality time, medical emergencies, or if you had kids?
- Just be yourself. In the wise words of Dave Grohl, “No one is you and that is your biggest power”. You might be surprised who falls in love with you – the real you. In the mess and glory of your full humanity. Even Joker has his Harley Quinn, so that gives me hope.
“In the wise words of Dave Grohl, “No one is you and that is your biggest power”. You might be surprised who falls in love with you – the real you. In the mess and glory of your full #humanity.” #spoonie #ChronicIllness #disability #dating
Share on X
- Know that you will face rejection, and be okay with that. Whilst we might face more romantic rejections than an abled individual, there is an upside to that as well – we only get to be with the best sorts of people on this planet. In that sense, chronic illness is an automatic filter that sifts out the bad eggs.
- Know your self-worth. It is also important to be aware of your self-worth at all times – whether you’re single or in a relationship. Ironically, it was chronic illness that forced me to hone this awareness through acceptance. Self-acceptance isn’t an admission of failure; rather, it asks us to put our ego aside in order to unlock possibilities, be at peace, and regain a sense of freedom.
Pin to Your Dating, Disability & Chronic Illness Boards:
-
Read Related Posts:
- Loss of Identity with Chronic Illness & The Plot Twist: Sharpened Self-Worth
- How to Have a Healthy Relationship with Your Body (Even with Chronic Illness)
- Chronic Illness Quotes to Inspire, Motivate, Grieve, Hope & Laugh About
- There’s No One Way to Live Your Life
- Keeping Up with the World: Why it’s Important Despite Pain
Dating Tips & Insights for Potential Partners
So, someone interesting has caught your eye. You think that they may be your ‘type’ of person. The ‘problem’? They have a long-term illness or disability. This section addresses some questions you may have, but are unsure who to ask, or if it’s appropriate to ask. I will try to be as unbiased as I possibly can.
- Understand that there is no perfect partner or relationship. Every single person brings a new dynamic to a relationship. There are pros and cons to each dynamic. Decide what matters most to you most.
“There is no #perfect partner or #relationship. Every single person brings a new dynamic to a relationship. There are pros and cons to each dynamic. Decide what matters most to you most.” #DatingTips #ChronicIllness #RelationshipGoals
Share on X
- Don’t ghost. What’s up with ghosting these days? This is my number one pet peeve when it comes to dating in general. If you decide that it’s not going to work out, do the courtesy of letting the other party know, so they get some closure. Why lead someone on before disappearing into the ether?
-
Shift your perspective. Something interesting my ex-turned-boyfriend-again said to me: “Your chronic illnesses have some advantages, too. It enables me to have my own space, alone time, and time for other friends”.
I’m always happy to oblige because it means I get some me-time as well, without feeling pressured to do ‘coupley things’. Don’t get me wrong. Coupley things are important, as they generate memories and build bonds. But as a person with chronic pain and fatigue, my energy bar is limited, and I need more downtime than others.
Another caveat – said boyfriend is older now, so he’s seeking different experiences in life as well. Age does play a part to an extent. In a sense, his body has ‘caught up’ a little with mine. Whilst he’s definitely still a social creature, he also appreciates time at home a little more now. So we watch films and play chess at home, and go out for the occasional brunch, party or exhibit.
Conclusion to Dating with Chronic Illness
This article is a sum of my experiences in regards to dating with chronic illness and disability thus far, but the story hasn’t ended yet. (Does it ever end, really?) I am still learning as I go along, and will add to this post should I gain any other insights.
I would also love to hear about your experiences in regards to dating with chronic illness or disability. What were your best and worst experiences, and why? If you’re happily married, how do you make it work? I would love to learn more from you as well!
And finally, if you’re an able-bodied individual, I’d love to hear your thoughts, questions and concerns as well. You can post an anonymous comment if that makes you feel more comfortable. I promise to be as open-minded and non-judgemental as I can. I believe in open, proactive discussion, as opposed to allowing misconceptions or fears to fester in the dark closet of your mind.
Happy dating to one and all – I hope you find your special person ♥️
If you liked this article, sign up for our mailing list so you don’t miss out on our latest posts! You will also receive an e-book full of uplifting messages, quotes and illustrations, as a token of appreciation!
-
Read Related Posts:
- 7 Reminders For Those Bad Days to Keep You Going
- My Responses to “A Day in the Life” Linkup (What Does ‘Normal’ Even Mean?)
- “It’s in My Blood”: Featuring People with Illnesses, Passions & Talents
- 7 Ways to Be a Better Friend to Someone with a Chronic Illness (and 3 Things You Should Never Do)
- A Page From a Sick Girl’s Diary: Sometimes I Wish I was an Old Person
Pin to Your Dating with Chronic Illness & Disability Boards:
Easy Gluten-Free Finger Foods Everyone Will Love
Are you looking for gluten-free finger foods for your next party that everyone will enjoy? We have you covered! Preparing gluten-free party bites doesn’t have to be complicated. Whether you’re hosting a Superbowl party, game night, baby shower, bridal shower, or holiday gathering, this collection […]
mind-&-emotionsAre you looking for gluten-free finger foods for your next party that everyone will enjoy? We have you covered! Preparing gluten-free party bites doesn’t have to be complicated. Whether you’re hosting a Superbowl party, game night, baby shower, bridal shower, or holiday gathering, this collection of easy gluten-free appetizers will make entertaining a breeze.

Who says gluten-free party food recipes aren’t as tasty as traditional options. These simple gluten-free snacks are so delicious, even the toughest critics won’t know the difference. From buffalo wings and spicy deviled eggs, to pretzel dogs and pizza rolls, get ready to be the host with the most.
Many of these dishes use naturally gluten-free ingredients and require minimal preparation. So not only are these gluten-free finger foods tasty but they’re convenient too.
Are you ready to be blown away? Let’s go.





























You May Also Want To Read
30+ Amazing Gluten-Free Soup Recipes to Warm Up Your Fall and Winter
30+ Delicious Dairy and Gluten-Free BBQ Side Dishes to Try This Summer
100+ Gluten-Free and Dairy-Free Mother’s Day Recipes
19 Gluten-Free Valentines Treats to Make for Your Sweetie
Summary
If you’re looking for crowd-pleasing gluten-free party snacks, this roundup won’t disappoint. Try 1, 2 or a few and watch how quickly these tasty gluten-free bites disappear. Who knows, you just might find some new go-to favorites. Happy hosting!
The post Easy Gluten-Free Finger Foods Everyone Will Love appeared first on Health Uprising Now.
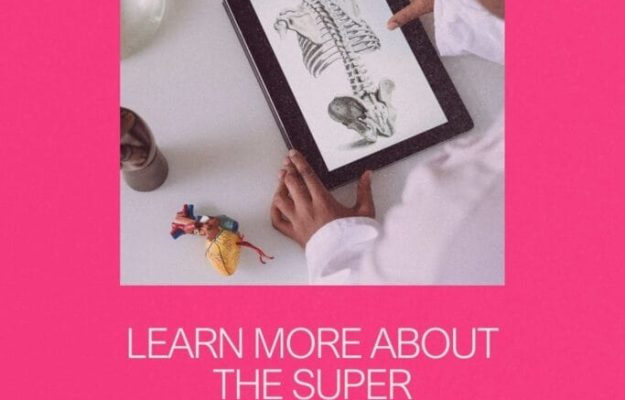
My Personal Experiences with Epiphrenic Esophageal Diverticulum (Plus Tips to Help Cope)
Two New Diagnoses – Epiphrenic Esophageal Diverticulum & Mitral Valve Stenosis Whilst I haven’t heard much good news in a long time, I did not expect 2025 to be a harbinger of such terrible news. It seems like I will need to get two major […]
Chronic voicesTwo New Diagnoses – Epiphrenic Esophageal Diverticulum & Mitral Valve Stenosis
Whilst I haven’t heard much good news in a long time, I did not expect 2025 to be a harbinger of such terrible news. It seems like I will need to get two major surgeries done, one for a severe mitral valve stenosis, and the other for an epiphrenic esophageal diverticulum. Well technically, epiphrenic esophageal diverticula, since there are two of them. Oh, and I also broke my molar tooth on Christmas Eve, so that was a bonus.
*Disclaimer: This article is meant for educational purposes, and is based on my personal experiences as a patient. Whilst I have done my utmost to be meticulous in research, I am not a doctor, and nothing in this article should be substituted for medical advice. Please consult your own doctor before changing or adding any new treatment protocols. This post may also contain affiliate links. It will cost you nothing to click on them. I will get a small referral fee from purchases you make, which helps with the maintenance of this blog. Read our Privacy Policy page for more information. Thank you!
Pin to Your Epiphrenic Esophageal Diverticulum & Rare Disease Boards:
-
Read Related Posts:
- Learn More About the Super Rare Disease – Esophageal Diverticulum
- My Second Brush with Death: A Broken Heart (Literally)
- What’s it Like to Live with a Heart Rhythm Disorder?
- MediSearch Review: A Medical AI Search Engine for Patients, Clinicians & Medical Writers
- Latest Research on Antiphospholipid Syndrome (2024 Edition)
Classifications for Esophageal Diverticulum
To be honest, the diagnosis for epiphrenic esophageal diverticulum scares me more than the mitral valve stenosis, only because it’s so rare. In practice, esophageal diverticulum is divided into a few different types of classifications from an anatomical and etiopathogenic point of view (Constantin et al., 2023). They are also subdivided based on their location. WebMD summarises the different types of esophageal diverticula here, although the classifications can get even more fine-grained than that (Whitten, 2024, February 20).
However, from what I’ve gathered after reading multiple medical journals, there is currently no agreed upon standard for treatment. Classifications for the disease itself are not even ‘finalised’, so to speak. Meaning there is no handbook or protocol for doctors or surgeons to refer to for this condition, and it’s mainly ‘play by ear’. Both my surgeon and doctor at the hospital have only seen one case in their career.
I’ll talk about the stenosis in a separate post, as I would like to focus on my diagnosis and symptoms for epiphrenic esophageal diverticulum in this one. This post is part of a two-part series. I will share my personal experiences in this one; you can find more research and facts on esophageal diverticulum in this post.
How I Learned About My Epiphrenic Esophageal Diverticulum
I reluctantly admitted myself to the A&E/ER one evening, as my forearm was bloated and swollen. It felt like my skin was going to burst. The only reason I had gone to the A&E was because the GP had assumed it was an abscess.
The rheumatology team saw me the next day, whilst I was snoozing along the corridor of a random ward. They were collectively certain that it was a blood clot, considering I have Antiphospholipid Syndrome, a blood clotting disorder. A few scans and tests later, they were all surprised that it wasn’t a blood clot, neither was it a fracture.
They did however, find some liquid near my lung, and the outpouching characteristic of esophageal diverticulum. According to Constantin et al. (2023), “somewhere between 0.06 – 4% [of epiphrenic esophageal diverticulum] are discovered incidentally, radiologically”.
The swollen arm and liquid in the lung subsequently resolved on their own. In fact, when they wheeled me in to do a pleural biopsy, they wheeled me back out as the surgeon said that ‘there was nothing to biopsy’. This is why I rarely rush to the A&E for every pain, even if extreme. Living with chronic illness means constant pain, and the occasional weird symptom.
My own rheumatologist said that the esophageal diverticula probably have been there for some time. He also said it was probably unrelated to my other autoimmune diseases, though I really beg to differ. I personally think it doesn’t make sense that none of my long list of medical conditions are related.
-
Read Related Posts:
- What it Feels Like to be Refused Treatment by a Hospital’s A&E / ER
- Tell Me You’re Chronically Ill Without Telling Me You’re Chronically Ill (51 Chronic Illness Memes)
- “But That’s Normal for Me” (Why I Mistook Dengue Fever for a Lupus Flare)
- 12 Visible Evidence of a Body Gone Rogue (Is Invisible Illness Truly Invisible?)
- Why I Need to See 10 Different Doctors on a Regular Basis
My Epiphrenic Esophageal Diverticulum Symptoms
According to Sato et al. (2023), the main symptoms of esophageal diverticulum are “dysphagia, regurgitation, weight loss, heartburn, respiratory complaints, and retrosternal pain when swallowing food”.
My own biggest problem was and is regurgitation, especially whilst asleep in the middle of the night. I wake to violent fits of coughing, as my esophagus tries to purge the food trapped within the pouches. Sometimes my throat is so irritated that I vomit. In fact, it happened twice again last night.
At first, I had simply assumed that it was GERD/acid reflux, as I am on long-term steroid therapy for Lupus and Sjögren’s disease. Plus I drink way too much coffee, and my eating habits are not the best (yes, sue me). When I received the diagnosis for epiphrenic esophageal diverticulum, everything made so much more sense.
Other symptoms I’ve had to date are: minor incidents of dysphagia (trouble swallowing food), and being really gassy. My digestive system makes a lot of weird noises, and I feel bloated and uncomfortable. These are sporadic with no fixed pattern. My doctor has said before that I probably have Irritable Bowel Syndrome (IBS) too, so I’m not sure what’s triggering what. Chronic illness comorbidities are fun like that.
In addition, my throat often feels scratchy, as if there are tiny specks of food trapped within it, plastered to the ‘walls’. There are ‘better’ and worse days as well. On the ‘better’ days, the symptoms are mostly quiescent with some minor coughing. On bad days, that ‘stuck’ feeling is there for almost 24 hours, and I am unable to eat without vomiting.
My Increase in Symptoms
The symptoms rapidly became worse over time. I am now being involuntarily woken almost every night by violent coughing, regurgitation and vomiting. On a ‘better’ night, I wake once or twice. On a ‘bad’ night, that would be at least every 2 hours.
Combine that with horrendous chronic urticaria that antihistamines barely alleviate, it means that I hardly get a good night’s sleep. In fact, that happened again last night, as I was up until 6am scratching and coughing.
Unsurprisingly, this isn’t great for my physical or mental health, as I feel extremely frayed at the edges, and completely worn out. What sort of life is this, if I am in pain and discomfort both day and night? What makes it even more depressing is that there is no medication to even relieve some of the symptoms either.
Pin to Your Epiphrenic Esophageal Diverticulum & Motility Disorder Boards:

-
Read Related Posts:
- Dysphagia & Swallowing Problems (and How Oral Vitamin Sprays Can be of Help to You)
- Depression After Knee Surgery & How to Cope
- Why Painkillers are One of My Biggest Allies for a Decent Quality of Life
- Why it Feels Like Suicide is an Option When You Live with Chronic Illness or Disability
- How Much Time Are You Wasting On Sleep?
More Information About Epiphrenic Esophageal Diverticulum
This section covers more about epiphrenic esophageal diverticulum specifically. You can read the research post for more information about esophageal diverticulum in general.
My two diverticula are mainly epiphrenic in nature (towards the tail end of the esophagus), although one is slightly higher up. Out of the various types of esophageal diverticulum, epiphrenic esophageal diverticulum comprises less than 10% of all cases, with an estimated incidence of 1:500,000 per year (i.e. 1 out of half a million people) (Abdollahimohammad et al., 2014). The most common is Zenker’s diverticulum, which occurs at the top end of the esophagus.
According to Alicuben et al. (2023), patients with epiphrenic esophageal diverticula are symptomatic only about 10% to 20% of the time. Symptoms tend to begin when the diverticulum becomes bigger than 5cm (Abdollahimohammad et al., 2014).
Having said that, both my epiphrenic esophageal diverticula are a little smaller than 5cm, and I have been progressively symptomatic. I’m unsure if that’s good or bad luck. Good because I guess, well, treating something earlier is usually better than later. Bad because the symptoms are obviously not fun.
The Complications of Epiphrenic Esophageal Diverticulum
Many symptoms of epiphrenic esophageal diverticulum are similar to other gastrointestinal and common medical conditions, such as acid reflux or side effects of NSAIDs. As a result, many patients with epiphrenic esophageal diverticulum are diagnosed late, which can lead to further complications, such as “gastrointestinal bleeding, aspiration pneumonia or cancer” (Conklin et al., 2009).
The incidence of cancer in patients with epiphrenic esophageal diverticulum is around 0.3% to 3%, and it is often at an advanced stage when discovered (Conklin et al., 2009; also see: Hjern et al., 2015). According to Constantin et al. (2023), there is also the risk of developing esophageal cancer, around 10 years after symptomatic esophageal diverticulum.
Some Other Characteristics of Epiphrenic Esophageal Diverticulum
According to Constantin et al. (2023) there is “no correlation between size and retentive character” for epiphrenic esophageal diverticulum in particular. That means that food and liquid can get stuck regardless of the size of the epiphrenic esophageal diverticulum, to give rise to symptoms.
In addition, “one of the early signs of food stasis in a pharyngeal-ED [esophageal diverticulum] is the appearance of hydro aerial noises when ingesting fluids”. As a result of food stasis, sialorrhea (hypersalivation) occurs (Constantin et al., 2023).
After reading that, I wondered if my drooling at night is a consequence of the epiphrenic esophageal diverticula. But as I need to wear a mouthguard for bruxism and TMJ disorder issues as well, I suppose it could be multifactorial.
Pin to Your Epiphrenic Esophageal Diverticulum & Rare Disease Boards:
-
Read Related Posts:
- How Does Antiphospholipid Syndrome Affect The Body? (Beyond the Blood to Major Organs)
- Oral Spray Vitamins: A Quick & Easy Way to Get Your Nutrients with Chronic Illness
- Sometimes, Physical Pain Isn’t the Worst Part About Chronic Illness
- How to Survive the Holidays When Chronic Illness & Disability Cause Pain
- 40 People with Chronic Illness Share Their Best Pain Management Tips (What to Do if an Unforeseen Pain Flare Hits)
Confirmation of My Epiphrenic Esophageal Diverticulum Diagnosis – a Barium Swallow Test
After the incidental finding of the epiphrenic esophageal diverticulum, I was scheduled for a barium swallow test. This is one of the more definitive tests for esophageal diverticulum, and also certain motility disorders such as achalasia (Sudarshan et al., 2021).
I was made to drink a chalky liquid at intervals, as the medical team watched and timed the flow under fluoroscopy (a type of x-ray that shows the movement of organs in real-time) (MedlinePlus, 2024, August 27). The mixture tasted quite nice to me, a bit like yoghurt, but don’t take my word for it as the technician said that no one else likes it. The doctors’ biggest concern was achalasia, which the team decided that I did not have based on the test. They were also able to measure the size of the diverticula and gather other information from the barium swallow test.
Other Essential Preoperative Tests for Epiphrenic Esophageal Diverticulum
I will need to get surgery done in my surgeon’s opinion. Whilst it’s a fairly high-risk surgery, I am going to agree with him, as the symptoms are becoming unbearable and interferes with my life every day. Some preoperative tests will need to be done, namely an upper endoscopy and manometry.
Whilst the surgeon has said that the manometry might not be necessary since we’ll need to do a fundoplication (an anti-reflux procedure) during the Heller’s myotomy (surgery) regardless, I insist upon it. This is because epiphrenic esophageal diverticulum mostly stems from a motility disorder, so it is best to treat the underlying cause if so. Whilst the fundoplication might treat any existing motility disorder, I think it’s best to actually know what the disorder is, if there is indeed one.
According to Alicuben et al. (2023), “failure to identify and treat the underlying motility disorder during diverticulum resection has been associated with high rates of recurrence and leak along the staple line in the range of 10% to 20%.” They also state that, “specifically, failure to perform an adequate myotomy in such patients has yielded leak rates exceeding 25% when diverticulectomy alone is performed”.
You can learn more about these diagnostic tests, surgeries and why they’re important in the post here.
-
Read Related Posts:
- What It Feels Like to be Suddenly Disabled
- Knee Surgery for Spontaneous Bilateral Patellar Tendon Rupture: Weeks 1 – 6
- Wound Care & What to Wear After Knee Surgery
- The Annoying Thing About Living with Antiphospholipid Syndrome (My Personal Experiences)
- An Experience from Hell: Pulmonary Embolism, DVTs & Antiphospholipid Syndrome
General Symptom Management for Epiphrenic Esophageal Diverticulum
As mentioned, there is no medication to help with symptom relief, and the doctors don’t have much clue about it either. The advice I was given by the gastroenterologist was rather generic, and there aren’t many tips online either. The closest I have found for managing epiphrenic esophageal diverticulum are general esophageal soft food diet tips.
A list of esophageal soft food diet tips can be found on the Cedars Sinai (2018, May 30) website, and includes: eating slowly in small amounts, chewing thoroughly, drinking fluids whilst eating to flush the food down, sitting upright whilst eating and up to 60 minutes after, avoiding food 3 hours before sleeping, avoiding caffeinated beverages, avoiding tough meats, abrasive foods and breads with chewy textures, and to stop eating when you start to feel satiated. This is pretty much what the gastroenterologist has advised me to do for symptom management of my epiphrenic esophageal diverticula.
You may or may not have trouble digesting food in and of itself with epiphrenic esophageal diverticulum. However, many of the symptoms mimic those of esophageal cancer or a motility disorder. Thus, many of the symptom management tips closely resemble these diseases. It also largely depends on your personal symptoms, how and when it affects you. For instance, regurgitation whilst sleeping is my biggest symptom, so my management plan might look different from yours, if you mostly get dysphagia instead.
Dietary changes and eating times are primary ones, however. According to Yam et al. (2023, April 24), “if patients are not surgical candidates, then management with diet changes such as eating bland food and drinking water after every bite to help flush any food out of the diverticulum is recommended”.
Pin to Your Chronic Pain & Pain Management Boards:
How I’m Personally Managing My Epiphrenic Esophageal Diverticulum Symptoms
It’s been a lot of trial and error for me, personally. I have a rough idea of which types of food cause the most damage, having learned the painful way. By sharing these personal experiences, I hope that it saves you some pain.
There are also a few things I want to try but have yet to do them regularly, so I’ll update the post after I’ve experimented with them a bit more. One thing I’d like to try is stretching to aid with digestion, and make it a nightly routine. It seems safe and simple enough to try and implement.
Dietary & Lifestyle Changes
I rarely eat at regular timings, so I’m trying to work on that. I think it’s helped a little, mainly because there is less acid reflux, which can also contribute to irritation along the digestive tract – which includes the esophagus.
The most painful episode for me so far was eating a bag of risotto chips at night, because I thought that rice crackers would be less abrasive and easier to digest than potato or corn chips. I was proved so terribly wrong, as I was up all night coughing and vomiting every 2 hours, and even the entire day after as well. I now have a phobia of anything crunchy, and avoid them especially at night.
Food Textures Matter a Great Deal
I’ve found that foods that are either crunchy or flaky to be the worst, and also anything with lots of ‘specks’ in it, such as black peppercorns.
I probably don’t have to explain ‘crunchy’ to you – stuff like crisps, deep-fried chicken and certain cereals. ‘Flaky’ includes bread, sugary candies like soan papdi (which I love), ginger slices, and basically anything that can be broken down into strips, if that makes sense.
Bread, especially sliced bread with lots of ‘air pockets’ tends to be the worst. This is because they get chewed up into tiny specks that ultimately become trapped in the pouches of the esophageal diverticula. I can feel them tickle at my throat, begging to be spat out. And when they refuse to budge, my body reacts and expels them via vomiting.
The suggestion to ‘eat bland food’ does not appeal to me in the least bit, because I have also developed a phobia after only eating bland food for months on end whenever hospitalised. I call it ‘sick people food’, and the thought makes me depressed. However, the pain and discomfort from the esophageal diverticula means that sometimes, that’s worth the sacrifice.
Avoid Supper at All Costs, if Possible
My sleeping hours are very irregular, as one night of painsomnia can trigger a domino effect for days. So I tend to eat supper, especially if I hadn’t had much to eat earlier on in the day. Whilst the gastroenterologist did say not to eat 2 hours before sleeping, I find that I need to avoid eating right after dinner. It was difficult at first, because my body had been primed to want to eat at night. It’s much better now though. That little change does make a rather big difference.
I did try drinking fruit juice at night as I thought it was categorised as a ‘liquid diet’, but that didn’t work out too well for me at all. The fibre from the fruits tend to be like ‘strings’, so those get trapped in the esophageal diverticula pouches, too. According to Marcin (2024, March 25), such fruits are hard to digest because fibre “isn’t digested by your body”. Whilst the esophagus is technically before the digestive juices start their action, I guess this rule applies too, but in a different way. I’m learning as I go along.
Pin to Your Chronic Illness & Pain Management Boards:
Foods That are Fine for My Epiphrenic Esophageal Diverticulum
For more substantial meals, soups and stews (including stewed meat and vegetables), work best for me so far. As stews are boiled for a long period of time, this helps to break the food product down partially. In a gross metaphorical sense, they’ve been ‘pre-chewed’ a little to make things easier for you.
I eat less white rice than the average Asian, as it makes me feel quite bloated if I have too much of it. It is still a staple, and apart from bloating, doesn’t cause too much distress. I suppose that’s because they’ve been dehusked and are cooked, making them soft and less fibrous. Noodles and pasta are also okay in general, as once again, I guess it’s because they’ve been cooked at high temperatures.
Other foods I can tolerate with the epiphrenic esophageal diverticulum are: mashed potatoes, eggs, fish, spreads (like jams and compotes), any cooked meat or vegetable, and yoghurt. Things that are okay on the ‘naughty’ food list for me include: ice cream, marshmallow, bingsu (Korean shaved ice dessert), sorbet, jelly and custard.
Foods That Cause Pain for My Epiphrenic Esophageal Diverticulum
Foods that cause me the most pain, in hierarchical order, include: crisps/chips, sliced bread, cookies and biscuits, and high-fibre fruits. Whilst some of these foods can be quite plain, remember that it isn’t so much that your stomach has trouble digesting them. Rather, the pouches from the esophageal diverticula trap some food products more so than others. The time of consumption matters as well. So if I want to try my luck eating one of these food items, it’s safer to try it as early on in the day as possible.
Northwest Minimally Invasive Surgery (2021, April 20) has an information page for patients who have had esophageal or stomach surgery, but the advice is pretty relevant for epiphrenic esophageal diverticulum, too. They state that “it is important that foods consumed be smooth in texture to facilitate the movement of food through the swollen areas of the esophagus or stomach. Bread products that can expand with fluid are avoided entirely”. They also have a list of foods allowed and foods to avoid that makes total sense to me. The list is similar on the Cedars Sinai (2018, May 30) blog about esophageal dietary guidelines as well.
Experimenting with Supplements & Medications for Symptom Relief
I was suffering from two days of bloatedness and regurgitation a while back, and just randomly thought I’d try some magnesium. The justification being that magnesium is an essential mineral for the proper functioning of over 300 enzymes in the body, which includes muscle relaxation and digestion (Al Alawi et al., 2018).
I took a magnesium carbonate effervescent tablet, and was amazed to find that it helped to relieve the epiphrenic esophageal diverticulum symptoms a fair bit. I’m not sure how the esophagus is associated, but hey, it helped with some relief from two days of discomfort. Placebo or not, I’ll take it as a win, and something to add to my pain management toolkit. (I personally like the range of effervescent tablets from Voost.)
However, do note that this ‘trick’ isn’t fail-proof. Half the time it doesn’t work and I still wake up coughing and regurgitating. So I guess the magnesium simply aids with digestion and relaxation in general, which probably has an indirect effect on my body overall.
Interestingly, I did a search about it the next day, and found that magnesium supposedly helps some people who have achalasia. I couldn’t find any papers for it though, as esophageal diverticulum is a rare disease. Healthline has a list of the different types of magnesium supplements, which is interesting general knowledge (Hill, 2023, May 11).
Cough syrup also surprisingly seems to help with the non-stop coughing, even though it’s irritation from the esophagus, instead of the trachea/windpipe. I suppose it suppresses the urge to cough regardless? Having said that, both my parents are having an extremely bad cold and cough at the moment, so perhaps I’ve caught the bug, too. I’ll wait for a couple more weeks before concluding on the cough syrup relief.
Pin to Your Soft Food Diet & Chronic Pain Boards:
-
Read Related Posts:
- Vitamin D & Vitamin K2: How They Boost Each Other in the Body
- The Causes & Dangers of Malabsorption & An Easy Way to Get Your Nutrients
- The Lowdown on Medications and Antiphospholipid Syndrome (Warfarin, Enoxaparin, DOACs, NSAIDs & More)
- Physiotherapy After Knee Operation
- Is Yoga Accessible for People with Chronic Illness?
Conclusion on My Personal Experiences with Epiphrenic Esophageal Diverticulum
In sum, epiphrenic esophageal diverticulum is an extremely rare disease with limited research comparatively, so symptom and pain management are mostly through trial and error. Whilst it is not deadly in and of itself unless something rare happens (such as a rupture that will not stop bleeding), it tends to worsen over time. There is also a very small risk of esophageal cancer further down the road. It has definitely ruined my quality of life, especially with the regurgitation whilst sleeping at night. The dietary and lifestyle changes are annoying, because managing my other chronic illnesses is demanding enough.
Whilst I am certainly not looking forward to yet another high-risk surgery in a relatively short span of time, I really hope that I feel better after I recover from it. I’ve read a few Reddit threads on other patients’ experiences with Heller myotomy and fundoplication surgeries, and some of the aftereffects sound really painful and scary. But I guess I don’t really have much of a choice, do I?
If you’ve never had surgery or been chronically ill – the healing process is actually the worst, only because it’s the most boring, painful and helpless period. All you can do is wait for the pain to subside and the wounds to close, which can take months and sometimes, years. But I guess, hope for symptom relief is what keeps me, and others like me, going.
Learn More About the Super Rare Disease – Esophageal Diverticulum
-
Read Related Posts:
- Chronic Illness Quotes to Inspire, Motivate, Grieve, Hope & Laugh About
- “It’s in My Blood”: Sarah Frison – A Pastry Chef with a Stomach Disorder
- “It’s in My Blood”: Roy George – A Dramatic Life with a Short Bowel
- Fun Things To Do While Recovering From Surgery: Hobbies, Crafts & Games
- My Recovery Time for Simultaneous Bilateral Patellar Tendon Rupture (With Lupus & Steroid Treatment)
If you liked this article, sign up for our mailing list so you don’t miss out on our latest posts! You will also receive an e-book full of uplifting messages, quotes and illustrations, as a token of appreciation!
Pin to Your Epiphrenic Esophageal Diverticulum & Rare Disease Boards:
- Abdollahimohammad, A., Masinaeinezhad, N., & Firouzkouhi, M. (2014). Epiphrenic esophageal diverticula. Journal of Research in Medical Sciences : The Official Journal of Isfahan University of Medical Sciences, 19(8), 795–797. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4235103/
- Al Alawi, A. M., Majoni, S. W., & Falhammar, H. (2018). Magnesium and Human Health: Perspectives and Research Directions. International Journal of Endocrinology, 2018, 9041694. https://doi.org/10.1155/2018/9041694
- Alicuben, E. T., Luketich, J. D., & Levy, R. M. (2023). Epiphrenic Diverticulum. In Pryor, A. D. & Hawn, M. T. (Eds), Operative Techniques in Foregut Surgery (2nd ed.), 1. Wolters Kluwer Health. Retrieved from https://books.google.com.sg/books?id=xmGvEAAAQBAJ
- Cedars-Sinai. (2018, May 30). Esophageal Soft Food Diet Guidelines. Cedars-Sinai. https://www.cedars-sinai.org/blog/esophageal-soft-diet-guidelines.html
- Conklin, J. H., Singh, D., & Katlic, M. R. (2009). Epiphrenic Esophageal Diverticula: Spectrum of Symptoms and Consequences. Journal of Osteopathic Medicine, 109(10), 543–545. https://doi.org/10.7556/jaoa.2009.109.10.543
- Constantin, A., Constantinoiu, S., Achim, F., Socea, B., Costea, D. O., & Predescu, D. (2023). Esophageal diverticula: From diagnosis to therapeutic management—narrative review. Journal of Thoracic Disease, 15(2), 759–779. https://doi.org/10.21037/jtd-22-861
- Hill, A. (2023, May 11). 10 Types of Magnesium (and What to Use Each For). Healthline. https://www.healthline.com/nutrition/magnesium-types
- Hjern, F., Mahmood, M. W., Abraham-Nordling, M., Wolk, A., & Håkansson, N. (2015). Cohort study of corticosteroid use and risk of hospital admission for diverticular disease. British Journal of Surgery, 102(1), 119–124. https://doi.org/10.1002/bjs.9686
- Marcin, A. (2024, March 25). What Foods Are Easy to Digest? Healthline. https://www.healthline.com/health/easy-to-digest-foods
- MedlinePlus. (2024, August 27). Fluoroscopy. MedlinePlus. https://medlineplus.gov/lab-tests/fluoroscopy/
- Northwest Minimally Invasive Surgery. (2021, April 20). Esophageal Soft Food Diet. Northwest Minimally Invasive Surgery. https://www.northwestmis.com/procedure/esophageal-and-stomach/esophageal-soft-food-diet/
- Sato, Y., Tanaka, Y., Ohno, S., Endo, M., Okumura, N., Takahashi, T., & Matsuhashi, N. (2023). Optimal surgical approaches for esophageal epiphrenic diverticulum: Literature review and our experience. Clinical Journal of Gastroenterology, 16(3), 317–324. https://doi.org/10.1007/s12328-023-01765-2
- Sudarshan, M., Fort, M. W., Barlow, J. M., Allen, M. S., Ravi, K., Nichols, F., Cassivi, S. D., Wigle, D. A., Shen, R. K., & Blackmon, S. H. (2021). Management of Epiphrenic Diverticula and Short-term Outcomes. Seminars in Thoracic and Cardiovascular Surgery, 33(1), 242–246. https://doi.org/10.1053/j.semtcvs.2020.08.017
- Whitten, C. (2024, February 20). What to Know About Esophageal Diverticulum. WebMD. https://www.webmd.com/digestive-disorders/esophageal-diverticulum
- Yam, J., Baldwin, D. L., & Ahmad, S. A. (2023, April 24). Esophageal Diverticula. In StatPearls [Internet]. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK532858/
References:
Learn More About the Super Rare Disease – Esophageal Diverticulum
Why am I Writing About the Rare Disease, Esophageal Diverticulum? The short answer is because I was recently diagnosed with it, although symptoms have been accumulating for some time now. I had simply assumed that all the regurgitation and vomiting, even in the middle of […]
Chronic voicesWhy am I Writing About the Rare Disease, Esophageal Diverticulum?
The short answer is because I was recently diagnosed with it, although symptoms have been accumulating for some time now. I had simply assumed that all the regurgitation and vomiting, even in the middle of the night, were due to acid reflux.
If not for an admission to the A&E/ER for something completely unrelated, the doctors would never have found it. The esophageal diverticulum was an incidental finding after I did a CT scan. According to Constantin et al. (2023), “somewhere between 0.06 – 4% [of epiphrenic esophageal diverticulum] are discovered incidentally, radiologically”.
Anyway, I have decided to split this into a two part series. I will publish more about my personal experiences with epiphrenic esophageal diverticulum soon. This post will focus entirely on research I’ve done thus far, as a patient.
*Disclaimer: This article is meant for educational purposes, and is based on my personal experiences as a patient. Whilst I have done my utmost to be meticulous in research, I am not a doctor, and nothing in this article should be substituted for medical advice. Please consult your own doctor before changing or adding any new treatment protocols. This post may also contain affiliate links. It will cost you nothing to click on them. I will get a small referral fee from purchases you make, which helps with the maintenance of this blog. Read our Privacy Policy page for more information. Thank you!
-
Read Related Posts:
- What it Feels Like to be Refused Treatment by a Hospital’s A&E / ER
- What It Feels Like to be Suddenly Disabled: Taking on the Eye of the Tiger in the Year of the Tiger
- “But That’s Normal for Me” (Why I Mistook Dengue Fever for a Lupus Flare)
- 12 Visible Evidence of a Body Gone Rogue (Is Invisible Illness Truly Invisible?)
- Tell Me You’re Chronically Ill Without Telling Me You’re Chronically Ill (48 Chronic Illness Memes)
Pin to Your Rare Disease & Chronic Illness Boards:

A Brief Look at the Esophagus / Oesophagus
In order to understand what certain terms mean and the implications of the different types of esophageal diverticulum, we first need to understand a bit about how the esophagus works. The esophagus is the “hollow, muscular tube that carries food and liquid from your throat to your stomach”, and is part of your digestive system (Cleveland Clinic, 2021b, August 4). It is approximately 9 to 10 inches long (23 to 25 cm).
The esophagus itself is made up of four layers – the mucosa, submucosa, muscularis and adventitia (Yam et al., 2023, April 24), and can be divided into three anatomical segments – cervical, thoracic and abdominal (Chaudhry and Bordoni, 2023, July 24).
Peristalsis
The main function of the esophagus is to transport food from the mouth to stomach, and it does that through a series of muscular contractions known as peristalsis, which is an automatic wave-like movement that happens within the digestive tract (Chaudhry and Bordoni, 2023, July 24; Cleveland Clinic, 2022, April 28).
According to Nehra et al. (2022), “the proximal one-third of the esophagus is composed of striated muscle, the distal one-third is composed of smooth muscle, and the middle one-third contains a mixture of striated and smooth muscle”.
Peristalsis in the different muscle types is controlled by different types of neuronal activity. The lower esophageal sphincter is also made up of smooth muscle segments. This allows for the smooth passing of food into the stomach, and also prevents gastroesophageal reflux (Nehra et al., 2022).
Some other keywords in relation to the esophagus are:
- Esophageal lumen – the inside of the esophagus
- Esophageal sphincter – a ring-shaped muscle that contracts and expands</li
- Mediastinum – The centre area of the chest between the lungs, where the esophagus, heart, thymus, trachea and other structures can be found (Cleveland Clinic, 2022b, August 29)
What is Esophageal Diverticulum?
Esophageal diverticulum is a rare disease with a prevalence of less than 1% globally (Yam et al., 2023, April 24). Patients with esophageal diverticulum have an outpouching within the esophagus, and the disorder is categorised based on anatomical location and type. ‘Diverticula’ is the plural term, where there are more than one diverticulum.
Esophageal Diverticulum Based on Anatomical Location
There are primarily three types of esophageal diverticula – Zenker’s, mid-esophageal and epiphrenic, running from top to bottom of the esophagus (Constantin et al., 2023).
Within the pharyngoesophageal space, they can be further categorised as – Zenker’s, Killian-Jamieson and Laimer’s, once again based on where they occur (Watanabe et al., 2023). Here is a great illustration that shows the differences between these three types of diverticulum, from a left lateral and posterior view (Zakaria and Barawi, 2020).
Then there is also a diffuse type, known as “diffuse intramural pseudodiverticulosis” (DEIPD) (Constantin et al., 2023), which is a “chronic, fibrosing inflammatory disease” (Hentschel, 2022). Iatrogenic diverticulum has also been added as a category recently. As its name suggests, it happens post treatment – peroral endoscopic myotomy (POEM)-type endoscopic therapy, in this instance. Such treatments are often used for late complications of achalasia (a swallowing disorder) (Constantin et al., 2023).
Whilst esophageal diverticulum is a rare disease, the most common tends to be Zenker’s diverticulum – the one that occurs at the top of the esophagus. Esophageal diverticula are also more commonly found in the elderly, and in men as opposed to women (Yam et al., 2023, April 24), so I guess that makes me one lucky dark unicorn again.
Esophageal Diverticulum by Type
There are two ways that an esophageal diverticulum forms – pulsion or traction, with the former being more common. ‘Pulsion’ simply means pushing, whilst ‘traction’ means pulling. Therefore, pulsion diverticula push against the esophageal wall, whereas traction diverticula are ‘sucked in’, which lead to the formation of indentations in the esophageal wall (Cleveland Clinic, 2023, September 29).
According to Sato et al. (2019), pulsion esophageal diverticula form due to “inadequate relaxation of either the upper esophageal sphincter (UES) or the lower esophageal sphincter (LES), causing an increase of intraluminal pressure resulting in a herniation of the esophageal wall in an area of low parietal resistance”. Traction esophageal diverticula on the other hand, involves “adhesion and traction on the esophageal wall in the presence of a mediastinal inflammatory focus, resulting in the formation of a diverticular pouch”.
To simplify that explanation, a pulsion esophageal diverticulum is due to pressure within the esophagus. This leads to an abnormal bulge in the weaker areas of the esophageal wall. Traction esophageal diverticulum on the other hand, is caused by inflammation within the mediastinum. This pulling effect leads to the formation of pouches within the esophagus.
True Versus False Diverticula
Esophageal diverticulum can be further classified as either ‘true’ or ‘false’. According to Yam et al. (2023, April 24), true diverticula involve all four layers of the esophageal wall, whereas only the mucosa and submucosa layers are involved in false diverticula.
True diverticula are caused by traction (pulling), whilst false diverticula by pulsion (pushing). In general, Zenker’s and epiphrenic diverticula are false diverticula, whilst mid-esophageal diverticula are true diverticula.
Some Charts for Easier Digestion (Pun Not Quite Intended)
You can view the correlation between esophageal typography, anatomo-clinical criteria and etiopathogeny in Table 2 here (Constantin et al., 2023).
Figure 1 in this paper by Sudarshan and Murthy (2021) also provides an excellent summary of the three main types of esophageal diverticula. It includes their varying pathophysiology, presentations, work-up and management for easy comparison.
Finally, you can view some images of how various esophageal diverticula look like on Radiopaedia (Rezaee, 2024, December 17).
Pin to Your Rare Disease & Medical Infographic Boards:
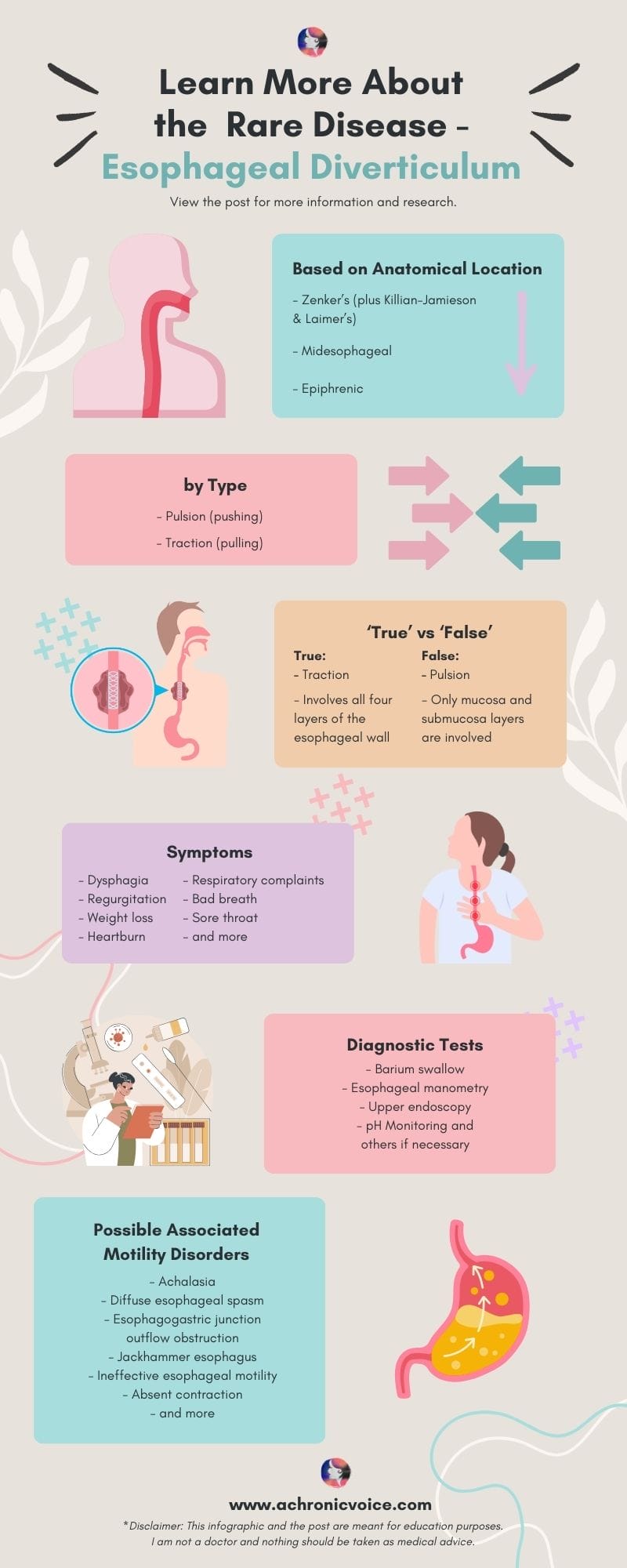
Esophageal Diverticulum Symptoms – From Mild to Severe
According to Sato et al. (2023), the main symptoms of esophageal diverticulum are “dysphagia, regurgitation, weight loss, heartburn, respiratory complaints, and retrosternal pain when swallowing food”.
The ‘milder’ symptoms of esophageal diverticulum include an irritating sensation in the throat as if something is stuck there, a sore throat and halitosis (bad breath). As the diverticulum increases in size over time, it can lead to other complications as food gets stuck in the pouches. For instance, patients can get “esophagitis, bleeding from ulceration, impaction, and stasis with regurgitation” (Sato et al., 2023).
Aspiration pneumonia can also happen especially when a person is asleep, where regurgitated food gets inhaled into the lungs and becomes infected. Apart from gastric content, the aspirated fluid can also consist of oropharyngeal secretions and particulate matter (Sanivarapu et al., 2024, March 20).
Aspiration pneumonia is also one of my biggest fears, as regurgitation at night is one of my main symptoms. According to Thomas et al. (2001), other serious manifestations of esophageal diverticulum include: “acute dyspnoea and stridor from pulmonary displacement, cardiac tachydysrhythmias from atrial compression and diverticular rupture, and, rarely, tension pneumothorax”.
In sum, esophageal diverticulum can potentially affect your heart, lungs, and their surrounding structures, due to pressure and/or rupture. It can also give rise to heart rhythm issues.
Whilst the formation of ulcers rarely leads to perforation or bleeding, such events can be life-threatening if they do happen. In addition, atypical symptoms of esophageal diverticulum may remain unknown until surgery is being done (Thomas et al., 2001).
-
Read Related Posts:
- Dysphagia & Swallowing Problems (and How Oral Vitamin Sprays Can be of Help to You)
- How Does Antiphospholipid Syndrome Affect The Body? (Beyond the Blood to Major Organs)
- An Experience from Hell: Pulmonary Embolism, DVTs & Antiphospholipid Syndrome
- My Second Brush with Death: A Broken Heart (Literally)
- What’s it Like to Live with a Heart Rhythm Disorder?
Diagnosing Esophageal Diverticulum
After that incidental finding of the esophageal diverticula from the CT scan, I had to go for a barium swallow test. The surgeon has also mentioned that I will need to do a manometry and endoscopy as pre-operative procedures.
This is in line with what I have read up thus far within the medical literature. According to Herbella and Patti (2012), the preoperative workup for esophageal diverticulum treatment includes: a barium swallow test, endoscopy, manometry, and pH monitoring if deemed necessary (also see: Thomas et al., 2001).
Let’s take a look at these tests used to diagnose esophageal diverticulum and motility disorders, to better understand why they’re important.
Barium Swallow Test
In order to clearly see and define the esophageal diverticulum, a barium swallow test (esophagram) (MedlinePlus, 2024a, August 27) is usually carried out first. The patient will be made to drink a chalky liquid at intervals. This helps with the visualisation of the diverticulum by ‘highlighting’ it under fluoroscopy, which is a type of x-ray that shows the movement of organs in real-time (MedlinePlus, 2024b, August 27). From the test, your medical team will then be able to determine the size and location of the diverticulum, and also if they are on the right or left side of the esophagus (Sudarshan et al., 2021).
The information from the barium swallow test is important for determining the course of treatment, and type of surgical method to use. In general, surgery is avoided for asymptomatic patients due to the risks, although some surgeons think that it is still essential, as up to 45% of patients demonstrated aspiration (Sudarshan et al., 2021). Some also think surgery is necessary, due to the “risk of cancerization of the diverticulum mucosa or spontaneous rupture” (Sato et al., 2023).
In addition, a timed barium swallow test is able to detect certain motility disorders such as achalasia, as well as “associated conditions such as dysmotility, hiatal hernia, distal esophageal rings, and reflux” (Sudarshan and Murthy, 2021).
Esophageal Manometry
According to Gyawali et al. (2020), “esophageal manometry is generally considered the gold standard for the diagnosis of motility disorders”. It is important to get this diagnostic test done especially for epiphrenic esophageal diverticula, as these are often due to an esophageal motility disorder, such as achalasia or diffuse esophageal spasm (Alicuben et al., 2023).
The word “manometry” simply means a measurement of pressure. A tube will be placed down your nasal cavity and into your esophagus. Thereafter, you will be made to swallow water and/or other liquids of different consistencies, in various bodily positions (Cleveland Clinic, 2023, October 5).
A high-resolution manometry is usually recommended, based on the latest research (Sato et al., 2019). The difference between a regular and high-resolution manometry is that the latter uses more catheters (36 as opposed to 5), thus producing more accurate results (Yadlapati, 2017).
Upper Endoscopy (Esophagogastroduodenoscopy)
A preoperative upper endoscopy is essential for several reasons. First, to rule out other possible diseases (such as Barrett’s esophagus) or malignancies (cancers), and also to clear any debris stuck in the diverticula before surgery is done (Alicuben et al., 2023; Herbella and Patti, 2012).
The Importance of Differential Diagnosis and Detection of Motility Disorders
There are a number of other disorders that can mimic an esophageal diverticulum, and vice versa. A differential diagnosis is essential to rule out such cases. This is simply a process that takes into account all possible diagnoses based on your individual symptoms, medical history, lifestyle and more (MedlinePlus, 2023, February 27). Additional tests may be done if deemed necessary. This helps your medical team to conclude with a more definitive diagnosis, and therefore, the treatment course to take.
For epiphrenic esophageal diverticulum, the differential diagnosis includes: “hiatal hernia, esophageal webs and strictures, esophageal duplication cyst, and esophageal carcinoma”. Other differential diagnosis of underlying causes should also be ruled out as well, such as: “achalasia, distal esophageal spasm, ineffective esophageal motility, esophagogastric junction outflow obstruction, end-stage gastroesophageal (GE) reflux disease with a “burnt out” esophagus, peptic stricture, or failed previous fundoplication” (Alicuben et al., 2023).
Whilst rare, it is also important to screen for malignancies (cancers). The incidence of malignancies from esophageal diverticula is 0.3% to 7% for pharyngoesophageal (which includes Zenker’s), 1.8% for midesophageal, and 0.6% for epiphrenic (Herbella and Patti, 2012).
The Link Between Motility Disorders and Esophageal Diverticulum
As mentioned, motility disorders are often the underlying cause of esophageal diverticulum – particularly so in epiphrenic esophageal diverticulum. In fact, according to Thomas et al. (2001), one should still “remain suspicious” even if a motility disorder is not detected during medical investigations, as apart from achalasia, most of such disorders “occur intermittently and may not be evident during oesophagoscopy, contrast radiology or standard manometry”.
Studies have also shown that “more than 75% of epiphrenic diverticula occur concomitantly with esophageal motility disorders” (Sato et al., 2019). In one small study by Nehra et al. (2002), all their patients with epiphrenic esophageal diverticulum were found to have a motility disorder, using 24-hour ambulatory motility testing.
Achalasia – The Most Common Motility Disorder Found in Esophageal Diverticulum
Achalasia has been mentioned numerous times in this post. Achalasia is a rare swallowing disorder that stems from damaged nerves in the esophagus, specifically in the lower esophageal sphincter. As a result, food and liquid are unable to move down to the stomach. How achalasia develops is still unknown, but has been purported to be autoimmune in nature (Cleveland Clinic, 2021a, April 6).
There are also different types of achalasia based on manometric patterns, namely: type 1 (classic), type 2, and type 3 (spastic). Type 1 achalasia has “minimal contractility in the esophageal body”, Type 2 has “intermittent periods of panesophageal pressurization”, and Type 3 has “premature or spastic distal esophageal contractions”. They also vary in immunohistochemical markers and histology (Patel et al., 2017).
Achalasia is also the most common motility disorder found in patients with esophageal diverticulum (Herbella and Patti, 2012). However, this is not the case in reverse. Less than 5% of patients with achalasia develop an epiphrenic esophageal diverticulum, with the exception of those with ‘vigorous’ achalasia, as more pulsion forces are involved (Thomas et al., 2001).
Diffuse Esophageal Spasm and Other Motility Disorders
The second most common motility disorder found in patients with epiphrenic esophageal diverticulum is diffuse esophageal spasm (Herbella and Patti, 2012). This is characterised by “simultaneous, uncoordinated, or rapidly propagated contractions that are of normal amplitude and accompanied by dysphagia”. Once again, differential diagnosis is critical because there is a long list of disorders that resemble it (Goel and Nookala, 2023, July 2).
In one small study using high-resolution impedance manometry, other motility disorders associated with esophageal diverticulum include, in descending order of occurrence: esophagogastric junction outflow obstruction, jackhammer esophagus, ineffective esophageal motility and absent contraction (Yuan et al., 2024). Another small study by Carlson et al. (2016), which also used high-resolution manometry, revealed “propagating peristalsis, often with hypercontractility” as the predominant motility pattern in their participants.
I would recommend reading this paper by Nehra et al. (2022), which has some insightful explanations of the different types of motility disorders. There are tables which detail how they appear on diagnostic tests, their differentiating features, and the recommended examinations and treatments.
It is also important to note that motility disorders can stem from different dysfunctions. For instance, it could arise from an autoimmune disease (e.g. Scleroderma), impaired inhibitory innervation (e.g. distal esophageal spasm), or excessive cholinergic stimulation (e.g. hypercontractile/jackhammer esophagus) (Nehra et al., 2022).
In sum, it is important to be sure that what you have is truly an esophageal diverticulum, as the treatment and management plan can be quite different for each diagnosis. And since a motility disorder is often the underlying cause of epiphrenic esophageal diverticulum, it is important to investigate this further in order to reduce or eliminate the chance of recurrence.
-
Read Related Posts:
- Antiphospholipid Syndrome Diagnosis: The A to Z Guide as a Patient
- Oral Spray Vitamins: A Quick & Easy Way to Get Your Nutrients with Chronic Illness
- The Causes & Dangers of Malabsorption & An Easy Way to Get Your Nutrients
- “It’s in My Blood”: Roy George – A Dramatic Life with a Short Bowel
- “It’s in My Blood”: Sarah Frison – A Pastry Chef with a Stomach Disorder
Pin to Your Rare Disease & Motility Disorder Boards:
Esophageal Diverticulum Treatments
According to Varghese et al. (2007), “optimal surgical treatment is debated, mortality being 9% in the largest reported surgical series of 33 patients”. That’s not much data to go on. For epiphrenic esophageal diverticulum, the ‘traditional’ methods of treatment include: “transthoracic resection, long esophagomyotomy, and an antireflux procedure” (Varghese et al., 2007).
I won’t deep-dive into each treatment type here because honestly, I’m probably as clueless as you are. I think I’ve done sufficient research to ask my surgeon the questions I need to ask however, and his answers convince me that he knows what he is doing. So I will share only the treatments that piqued my interest initially, and also what I would personally need.
Diverticulum Peroral Endoscopic Myotomy (D-POEM)
I had read that diverticulum peroral endoscopic myotomy (D-POEM) is becoming more popular as a surgical method for esophageal diverticulum. It is a minimally-invasive procedure with various adaptations, but generally involves steps to create tunnels, dissect and reseal certain parts of the esophagus and its related muscles (Wang et al., 2020).
I was interested in D-POEM, because studies have shown that it has a high technical and clinical success rate, and also a low recurrence rate. It is also commonly used to treat achalasia and other motility disorders (Pelton et al., 2024). However, it has mostly been used for Zenker’s diverticulum, as compared to other types of diverticula (Mavrogenis and Bazerbachi, 2023).
In any case, I asked my surgeon about it. I didn’t quite understand his explanation of why it wouldn’t make sense to use it. He did say that the surgical treatment that I’d need would be the same regardless of diverticulum type however, which is a Heller myotomy.
Heller Myotomy and Fundoplication
Heller myotomy is the standard procedure used to treat achalasia, where the lower esophageal sphincter is cut to relieve pressure, so that food and liquid can pass through. Acid reflux can occur after a Heller myotomy, so a partial fundoplication may be done in addition (UCLA Health, n.d.).
A fundoplication is an anti-reflux surgical procedure, where a “gastric fold is wrapped around the distal esophagus which enforces the lower esophageal sphincter and prevents gastroesophageal reflux”. It can be either full (Nissen) or partial (Toupet, Dor or Thal) (Abdrabou et al., 2022, April 1).
A Dor fundoplication takes the frontal approach, whilst a Toupet or Thal fundoplication from the back (Abdrabou et al., 2022, April 1). The most common is a Dor fundoplication, where part of the stomach is wrapped over the front of the esophagus and stitched in place. Nissen fundoplication is rarely advised for patients with achalasia, as it can lead to issues with peristalsis (Northwestern Medicine, n.d.).
My surgeon also said that he would probably need to perform the surgery at two entry points, with one incision from near the abdomen. Since my right chest wall has been tunnelled through before in order to repair my mitral valve, a thoracic surgeon will be needed on the surgical team to help ‘navigate’ through the web of adhesions.
According to Torres-Villalobos and Martin-del-Campo (2013), “myotomy can be safely performed using open abdominal and thoracic approaches, and for more than two decades, it has also been done using laparoscopy and thoracoscopy”. I’m assuming that was what the surgeon meant when he was explaining it to me.
Potential Surgical Complications
The rate of symptom relief for esophageal diverticulum is between 85% to 100%, using standard treatments such as “laparoscopic myotomy, diverticulectomy, and fundoplication”. Having said that, the complication rate for the procedure itself is high (Herbella and Patti, 2012).
Some complications that can occur post-surgery include: “air leaks, septicemia and/or sepsis, mediastinitis, mediastinal empyema with or without fistula, mediastinal abscess, postoperative wound infection, and postoperative hemorrhage” (Onwugbufor et al., 2013).
Leaks are one of the more common complications post surgery, at a rate of up to 23%. My own surgeon has told me that a leak was his biggest concern. The mortality rate for the procedure reaches up to 7% as well (Herbella and Patti, 2012).
Your surgeon will most likely use a combination of procedures in order to treat you, based on several factors. Your individual anatomy needs to be accounted for, as well as the size and position of the esophageal diverticulum, comorbidities and more. Each surgical method has its own risks and merits. For instance, a left thoracotomy provides good access to an epiphrenic diverticulum, but is also associated with a high morbidity rate (up to 21% of patients had a leak), and a mortality rate of up to 11% (Herbella and Patti, 2012).
Here is a summarised table of optimal surgical treatments used to treat epiphrenic esophageal diverticulum from 17 published series (Sato et al., 2023).
-
Read Related Posts:
- Knee Surgery for Spontaneous Bilateral Patellar Tendon Rupture: Weeks 1 – 6
- Must Haves After Knee Surgery to Stay Comfortable in Bed
- Fun Things To Do While Recovering From Surgery: Hobbies, Crafts & Games
- Wound Care & What to Wear After Knee Surgery
- The Annoying Thing About Living with Antiphospholipid Syndrome (My Personal Experiences)
Conclusion – There is Still So Much More to Learn About Esophageal Diverticulum
I hope that this article has given you some insight into the rare disease, esophageal diverticulum. I talked about epiphrenic esophageal diverticulum a little more, as that has a direct impact on me.
Doing research has helped me to cope with the helplessness and numbness I am currently feeling. Whenever I discover a correlation between my symptoms and an explanation from a medical journal, I feel enlightened or triumphant. To say that “knowledge is power” is underrated. Knowledge is healing. And we don’t know enough as it stands.
-
Read Related Posts:
- Latest Research on Antiphospholipid Syndrome
- MediSearch Review: A Medical AI Search Engine for Patients, Clinicians & Medical Writers
- Useful Things to Do While on Bed Rest After Surgery: Education, Advocacy & Volunteering
- What’s It Like Going Back to School as an Adult with Disability and Chronic Illness
- When Autoimmune Disorder Ravages Your Face (and How That Led to My Body Dysmorphic Disorder)
- Suffering with a Rare Disease, Isaac Syndrome, as Told from a Male Perspective
If you liked this article, sign up for our mailing list so you don’t miss out on our latest posts! You will also receive an e-book full of uplifting messages, quotes and illustrations, as a token of appreciation!
Pin to Your Rare Disease & Chronic Illness Boards:

- Abdollahimohammad, A., Masinaeinezhad, N., & Firouzkouhi, M. (2014). Epiphrenic esophageal diverticula. Journal of Research in Medical Sciences : The Official Journal of Isfahan University of Medical Sciences, 19(8), 795–797. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4235103/
- Abdrabou, A., Kusel, K., & Knipe, H. (2022, April 1). Fundoplication. Radiopaedia. https://doi.org/10.53347/rID-35706
- Alicuben, E. T., Luketich, J. D., & Levy, R. M. (2023). Epiphrenic Diverticulum. In Pryor, A. D. & Hawn, M. T. (Eds), Operative Techniques in Foregut Surgery (2nd ed.), 1. Wolters Kluwer Health. Retrieved from https://books.google.com.sg/books?id=xmGvEAAAQBAJ
- Carlson, D. A., Gluskin, A. B., Mogni, B., Koo, J., Sood, R., Lin, Z., & Pandolfino, J. E. (2016). Esophageal diverticula are associated with propagating peristalsis: A study utilizing high-resolution manometry. Neurogastroenterology & Motility, 28(3), 392–398. https://doi.org/10.1111/nmo.12739
- Chaudhry, S. R., & Bordoni, B. (2023, July 24). Anatomy, Thorax, Esophagus. In StatPearls [Internet]. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK482513/
- Cleveland Clinic. (2021a, April 6). Achalasia: A Disorder of the Esophagus. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17534-achalasia
- Cleveland Clinic. (2021b, August 4). Esophagus. Cleveland Clinic. https://my.clevelandclinic.org/health/body/21728-esophagus
- Cleveland Clinic. (2022a, April 28). Peristalsis. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22892-peristalsis
- Cleveland Clinic. (2022b, August 29). Mediastinum. Cleveland Clinic. https://my.clevelandclinic.org/health/body/24113-mediastinum
- Cleveland Clinic. (2023a, September 29). Esophageal Diverticulum. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/16977-esophageal-diverticulum
- Cleveland Clinic. (2023b, October 5). Esophageal Manometry Test. Cleveland Clinic. https://my.clevelandclinic.org/health/diagnostics/4952-esophageal-manometry-test
- Constantin, A., Constantinoiu, S., Achim, F., Socea, B., Costea, D. O., & Predescu, D. (2023). Esophageal diverticula: From diagnosis to therapeutic management—narrative review. Journal of Thoracic Disease, 15(2), 759–779. https://doi.org/10.21037/jtd-22-861
- Goel, S., & Nookala, V. (2023, July 2). Diffuse Esophageal Spasm. In StatPearls [Internet]. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK541106/
- Gyawali, C. P., Carlson, D. A., Chen, J. W., Patel, A., Wong, R. J., & Yadlapati, R. H. (2020). ACG Clinical Guidelines: Clinical Use of Esophageal Physiologic Testing. Official Journal of the American College of Gastroenterology | ACG, 115(9), 1412. https://doi.org/10.14309/ajg.0000000000000734
- Hentschel, F. (2022). Chronic fibrosing esophagitis with diffuse esophageal intramural pseudo-diverticulosis. JGH Open, 6(5), 287–291. https://doi.org/10.1002/jgh3.12750
- Herbella, F. A. M., & Patti, M. G. (2012). Modern pathophysiology and treatment of esophageal diverticula. Langenbeck’s Archives of Surgery, 397(1), 29–35. https://doi.org/10.1007/s00423-011-0843-2
- Hjern, F., Mahmood, M. W., Abraham-Nordling, M., Wolk, A., & Håkansson, N. (2015). Cohort study of corticosteroid use and risk of hospital admission for diverticular disease. British Journal of Surgery, 102(1), 119–124. https://doi.org/10.1002/bjs.9686
- Mavrogenis, G., & Bazerbachi, F. (2023). Peroral endoscopic myotomy for Zenker’s diverticulum without tunneling. Endoscopy, 55, E946–E948. https://doi.org/10.1055/a-2127-7402
- MedlinePlus. (2024a, August 27). Barium Swallow. MedlinePlus. https://medlineplus.gov/lab-tests/barium-swallow/
- MedlinePlus. (2024b, August 27). Fluoroscopy. MedlinePlus. https://medlineplus.gov/lab-tests/fluoroscopy/
- MedlinePlus. (2023, February 27). Differential Diagnosis: Test. MedlinePlus. https://medlineplus.gov/lab-tests/differential-diagnosis/
- Nehra, D., Lord, R. V., DeMeester, T. R., Theisen, J., Peters, J. H., Crookes, P. F., & Bremner, C. G. (2002). Physiologic Basis for the Treatment of Epiphrenic Diverticulum. Annals of Surgery, 235(3), 346–354. https://journals.lww.com/annalsofsurgery/abstract/2002/03000/physiologic_basis_for_the_treatment_of_epiphrenic.6.aspx
- Nehra, A. K., Sheedy, S. P., Johnson, C. D., Flicek, K. T., Venkatesh, S. K., Heiken, J. P., Wells, M. L., Ehman, E. C., Barlow, J. M., Fletcher, J. G., Olson, M. C., Bharucha, A. E., Katzka, D. A., & Fidler, J. L. (2022). Imaging Review of Gastrointestinal Motility Disorders. RadioGraphics. https://doi.org/10.1148/rg.220052
- Northwestern Medicine. (n.d.). Heller Myotomy. Northwestern Medicine. Retrieved 22 January 2025, from https://www.nm.org/conditions-and-care-areas/treatments/heller-myotomy
- Onwugbufor, M. T., Obirieze, A. C., Ortega, G., Allen, D., Cornwell, E. E., & Fullum, T. M. (2013). Surgical management of esophageal diverticulum: A review of the Nationwide Inpatient Sample database. Journal of Surgical Research, 184(1), 120–125. https://doi.org/10.1016/j.jss.2013.05.036
- Patel, D. A., Lappas, B. M., & Vaezi, M. F. (2017). An Overview of Achalasia and Its Subtypes. Gastroenterology & Hepatology, 13(7), 411–421. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5572971/
- Pelton, M., Kahaleh, M., & Tyberg, A. (2024). Peroral Endoscopic Myotomy for the Management of Esophageal Diverticula: Tunneling Forward. Techniques and Innovations in Gastrointestinal Endoscopy, 26(1), 56–67. https://doi.org/10.1016/j.tige.2023.12.003
- Rezaee, A., Niknejad, M., & Weerakkody, Y. (2024, December 17). Epiphrenic diverticulum. Radiopaedia. https://doi.org/10.53347/rID-20707
- Sanivarapu, R. R., Vaqar, S., & Gibson, J. (2024, March 20). Aspiration Pneumonia. In StatPearls [Internet]. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK470459/
- Sato, H., Takeuchi, M., Hashimoto, S., Mizuno, K., Furukawa, K., Sato, A., Yokoyama, J., & Terai, S. (2019). Esophageal diverticulum: New perspectives in the era of minimally invasive endoscopic treatment. World Journal of Gastroenterology, 25(12), 1457–1464. https://doi.org/10.3748/wjg.v25.i12.1457
- Sato, Y., Tanaka, Y., Ohno, S., Endo, M., Okumura, N., Takahashi, T., & Matsuhashi, N. (2023). Optimal surgical approaches for esophageal epiphrenic diverticulum: Literature review and our experience. Clinical Journal of Gastroenterology, 16(3), 317–324. https://doi.org/10.1007/s12328-023-01765-2
- Sudarshan, M., Fort, M. W., Barlow, J. M., Allen, M. S., Ravi, K., Nichols, F., Cassivi, S. D., Wigle, D. A., Shen, R. K., & Blackmon, S. H. (2021). Management of Epiphrenic Diverticula and Short-term Outcomes. Seminars in Thoracic and Cardiovascular Surgery, 33(1), 242–246. https://doi.org/10.1053/j.semtcvs.2020.08.017
- Sudarshan, M., & Murthy, S. (2021). Esophageal Motility Disorders and Diverticula: Physiologic Implication and Surgical Considerations. Foregut, 1(3), 263–267. https://doi.org/10.1177/26345161211045613
- Thomas, M. L., Anthony, A. A., Fosh, B. G., Finch, J. G., & Maddern, G. J. (2001). Oesophageal diverticula. BJS (British Journal of Surgery), 88(5), 629–642. https://doi.org/10.1046/j.1365-2168.2001.01733.x
- Torres-Villalobos, G., & Martin-del-Campo, L. A. (2013). Surgical Treatment for Achalasia of the Esophagus: Laparoscopic Heller Myotomy. Gastroenterology Research and Practice, 2013(1), 708327. https://doi.org/10.1155/2013/708327
- UCLA Health. (n.d.). Esophageal Health – Esophageal / Heller Myotomy. UCLA Health. Retrieved 22 January 2025, from https://www.uclahealth.org/medical-services/gastro/esophageal-health/tests-treatments/surgical/esophageal-heller-myotomy
- Varghese, T. K., Marshall, B., Chang, A. C., Pickens, A., Lau, C. L., & Orringer, M. B. (2007). Surgical Treatment of Epiphrenic Diverticula: A 30-Year Experience. The Annals of Thoracic Surgery, 84(6), 1801–1809. tps://doi.org/10.1016/j.athoracsur.2007.06.057″ target=”_blank”>https://doi.org/10.1016/j.athoracsur.2007.06.057
- Wang, S., Chai, N., & Linghu, E. (2020). Diverticulum Peroral Endoscopic Myotomy (D-POEM). In Linghu, E. (Ed.), Therapeutics of Digestive Endoscopic Tunnel Technique (pp. 121–124). Springer. https://doi.org/10.1007/978-981-15-1998-7_9
- Watanabe, Y., Taniyama, Y., Koseki, K., Ishida, H., Ozawa, Y., Okamoto, H., Sato, C., Unno, M., & Kamei, T. (2023). Distinguishing Killian–Jamieson diverticulum from Zenker’s diverticulum. Surgical Case Reports, 9(1), 21. https://doi.org/10.1186/s40792-023-01599-7
- Yadlapati, R. (2017). High Resolution Manometry Vs Conventional Line Tracing for Esophageal Motility Disorders. Gastroenterology & Hepatology, 13(3), 176–178. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5439137/
- Yam, J., Baldwin, D. L., & Ahmad, S. A. (2023). Esophageal Diverticula. In StatPearls [Internet]. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK532858/
- Yuan, M.-C., Chou, C.-K., Chen, C.-C., Wang, H.-P., Wu, J.-F., & Tseng, P.-H. (2024). Characteristics of Esophageal Motility and Associated Symptom Profiles in Patients with Esophageal Diverticulum: A Study Based on High-Resolution Impedance Manometry. Digestive Diseases and Sciences, 69(2), 510–520. https://doi.org/10.1007/s10620-023-08196-6
- Zakaria, A., & Barawi, M. (2020). Endoscopic treatment of Killian-Jamieson diverticulum using submucosal tunneling diverticulotomy technique. VideoGIE, 5. https://doi.org/10.1016/j.vgie.2020.05.031
References:
Gluten-Free Christmas Dinner Recipes for a Delicious Holiday Feast
The Christmas season has arrived and so have these delicious gluten-free Christmas Dinner recipes. In this recipe roundup, you’ll find a collection of savory gluten-free Christmas main dishes to delight your guests and make your holiday meal unforgettable. Pair them with the delicious assortment of […]
mind-&-emotionsThe Christmas season has arrived and so have these delicious gluten-free Christmas Dinner recipes. In this recipe roundup, you’ll find a collection of savory gluten-free Christmas main dishes to delight your guests and make your holiday meal unforgettable. Pair them with the delicious assortment of gluten-free Christmas side dishes below and you’re sure to have a festive feast that everyone will enjoy.
Whether you’re hosting a big family gathering or enjoying an intimate dinner, these dishes will add warmth, flavor, and joy to your celebration.

My first gluten-free Christmas was depressing. Deprived of my favorite holiday recipes I ate a simple plate of rice, turkey, and maybe a vegetable. I had no idea of other festive foods I could enjoy. So I ate my meager plate while watching others enjoy their sumptuous selections.
Well no more sitting on the sidelines while everyone else enjoys the holiday feast. These gluten-free Christmas Dinner Recipes ensure you can savor every bite without worry!
While every effort has been made to curate only gluten-free recipes, always use caution and best judgment when following someone else’s recipe.
I recommend looking for the “gluten-free” label on items like chicken and beef broth, bacon, barbecue, and sriracha sauces. Although they may not contain flour, some brands can contain gluten. For more information, check out 10 Gluten Free Life Hacks.
Gluten-Free Christmas Dinner Recipes
GLUTEN-FREE CHRISTMAS MAIN DISHES














GLUTEN-FREE CHRISTMAS SIDE DISHES









Summary
Whether you’re hosting a gluten-free gathering or simply looking for delicious options to enjoy this holiday season, these gluten-free Christmas dinner ideas offer selections everyone will love. Mix and match them with our collection of gluten-free Christmas side dishes to create a complete and festive menu. With these recipes, you’ll be able to enjoy a delicious holiday feast without compromising on flavor or dietary needs. Happy holidays and happy eating!
The post Gluten-Free Christmas Dinner Recipes for a Delicious Holiday Feast appeared first on Health Uprising Now.
MediSearch Review: A Medical AI Search Engine for Patients, Clinicians & Medical Writers
Introduction to MediSearch, a Medical AI Search Engine You’ve probably asked ChatGPT, Gemini or another AI-powered chatbot a medical or health-related question before. Perhaps to try and find a diagnosis, or simply out of curiosity. I have personally asked them some medical questions that I […]
Chronic voicesIntroduction to MediSearch, a Medical AI Search Engine
You’ve probably asked ChatGPT, Gemini or another AI-powered chatbot a medical or health-related question before. Perhaps to try and find a diagnosis, or simply out of curiosity. I have personally asked them some medical questions that I already knew the answers to, simply to see how accurate they were. Google Gemini tends to skirt around health-related issues, whilst ChatGPT gives rather generic answers.
That is not necessarily a bad thing, because the scope of what these AI chatbots cover are quite broad. MediSearch on the other hand, is specifically built to focus on answering medical questions. Thus, you could say that it concentrates all of its resources on health-related topics, to give more detailed and accurate responses.
So when the founder of MediSearch, Eduard, approached me to write an honest review, I was excited to say the least. He also granted me access to the Pro version of MediSearch, so I could test the system and see the differences for myself. Let’s dive into the review – the good and bad (if any)!
*Disclaimer: Whilst this post is sponsored by MediSearch, all opinions expressed in this review are my own. This article is meant for educational purposes and is based on the author’s personal experiences. It is not to be substituted for medical advice. Please consult your own doctor before changing or adding any new treatment protocols. This post may also contain affiliate links. It will cost you nothing to click on them. I will get a small referral fee from purchases you make, which helps with the maintenance of this blog. Read our Privacy Policy page for more information. Thank you!
Pin to Your Medical AI & Health App Boards:
What is MediSearch Exactly, and is It Credible?
MediSearch is a medical AI-powered search engine with over a million users to date. It aims to be the world’s best medical Q&A system. It filters out the noise and only references credible sources and journals – so no random or woo-woo websites. ChatGPT and other AI chatbots are infamous for hallucinating, or to be more harsh, Scientific American straight up says they’re “bullshitting”.
MediSearch on the other hand, cites and links to all sources it derived its answers from. You can click on neatly arranged links to read the medical articles for yourself. If there are no credible sources to be found for your medical question, it will tell you so, or suggest potential questions you might be interested in instead.
One other thing that I love about MediSearch is that it is always up-to-date, so the answers it gives are all based on the latest scientific evidence. Its database is updated within hours of new publications. Even my favourite medical apps, such as MedScape (which I use to check for drug interactions), take weeks to prompt a manual update of medical information. To me, MediSearch truly taps into the power of AI to serve its purpose.
How MediSearch Works
If you’ve ever used ChatGPT or similar, then you know the drill. Simply ask MediSearch a medical question, and it quickly generates the answer with all sources cited. It differs from ChatGPT in the sense that you can’t simply type ‘tell me more’ like in a conversation, but it will suggest possible questions you can follow-up on.
I actually like that it does that, because it doesn’t guess what you’re trying to ask, which can lead you down rabbit holes. For example, I use ChatGPT quite a bit for coding work, but have realised that asking it questions in a conversational style often leads to errors. This is because it infers from the previous text, and amplifies its ‘understanding’ – which can often be false. Specificity is extremely important for medical questions, as it concerns you and your health.
Something else I like about MediSearch is the way its algorithm works. You don’t only get a summary of answers to your medical questions, but one that has been carefully crafted based on ranking factors such as journal quality, number of citations, and more. This means that the answers you’re getting are quality ones.
How Well Does MediSearch Perform for Medical Questions?
According to their website, MediSearch Pro has a 94% accuracy score when tested on the United States Medical Licensing Examination (USMLE) sample examination. The average score for a medical school graduate student taking the exam is 60%. Like me, you might be wondering what the USMLE is exactly, and I took the opportunity to ask MediSearch:
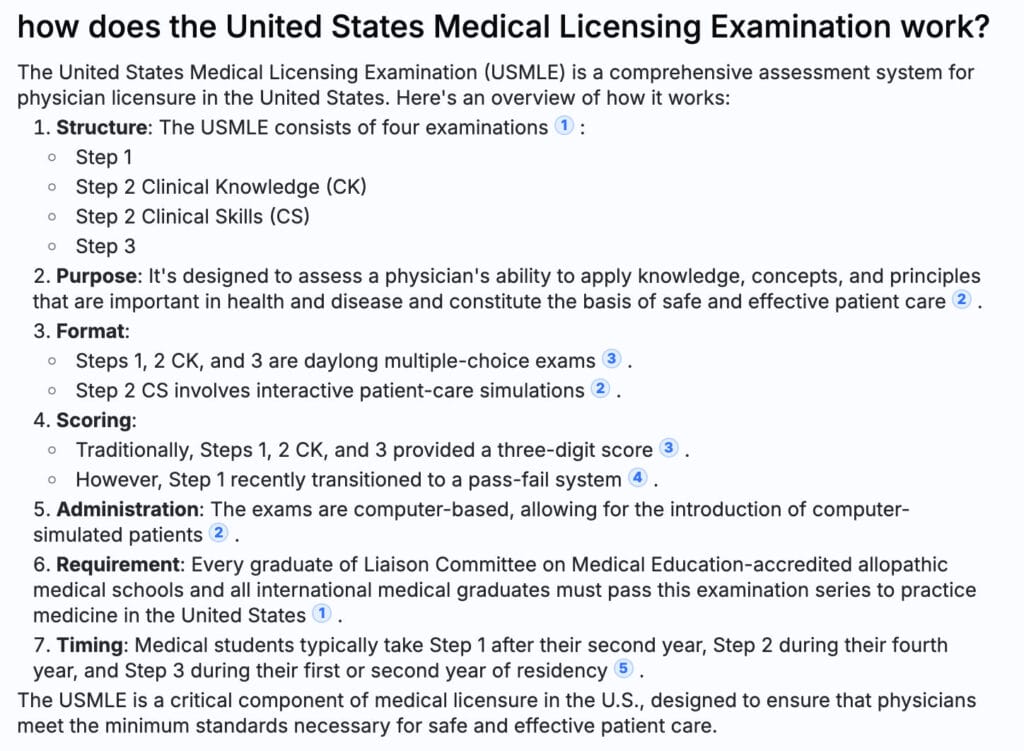
As you can see, the answer that MediSearch generated is comprehensive, and the information is broken down into a readable format that is easy to digest. The USMLE is an important exam that is compulsory for medical students to take, in order to practice medicine in the U.S.
When compared to other AI-powered search engines, MediSearch also had the highest accuracy score for the USMLE sample test, as can be seen from the chart below:
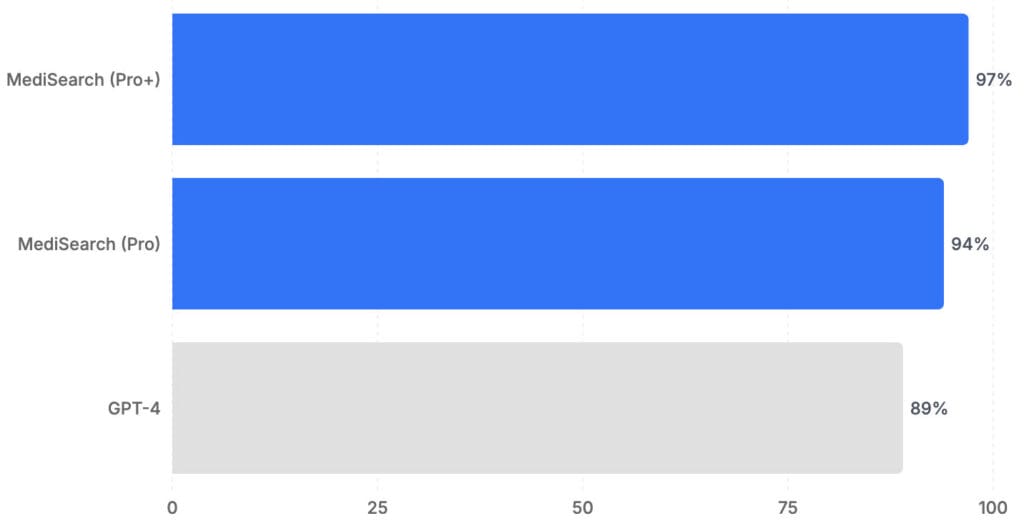
Taking MediSearch for a Test Drive
I decided to ask MediSearch questions I have done extensive research on as a patient, namely Antiphospholipid Syndrome (APS) and Spontaneous Bilateral Patellar Tendon Rupture (SBPTR). These are medical conditions I live with, and have written resources on myself.
Asking MediSearch a Basic Medical Question
I started with a basic question about APS, “What are the lab tests used for diagnosing Antiphospholipid syndrome?”:
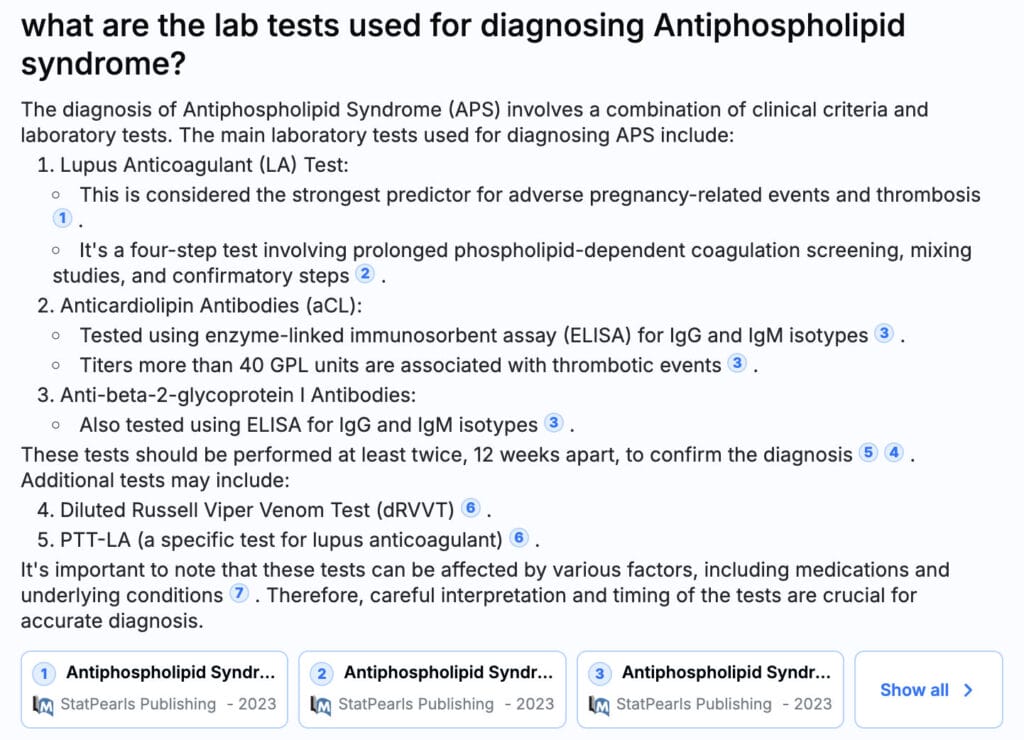
This pretty much summarises what took me hours of manual research, in order to include proper references for my APS resource guide. It also highlights that LA is “considered the strongest predictor for adverse pregnancy-related events and thrombosis”. This is an important note, and something my own rheumatologist has pointed out to me before.
Asking MediSearch a More Complex Medical Question
Next, I decided to ask MediSearch about Tecarfarin, which is a blood thinning medication still undergoing clinical trials. It is a drug that is targeted more for heart and kidney disease patients, and less for APS (a blood clotting autoimmune disorder), so I was curious as to what its response would be.
The response provided by MediSearch was well-informed once again, as seen in the screenshot below. It states clearly that Tecarfarin is still limited in evidence for APS, and tells me more about what it is, which stage the clinical trials are at, and more important medical information. This matches up with the research I had done (as a patient) for my article on medications in relation to APS, which took me months to put together.
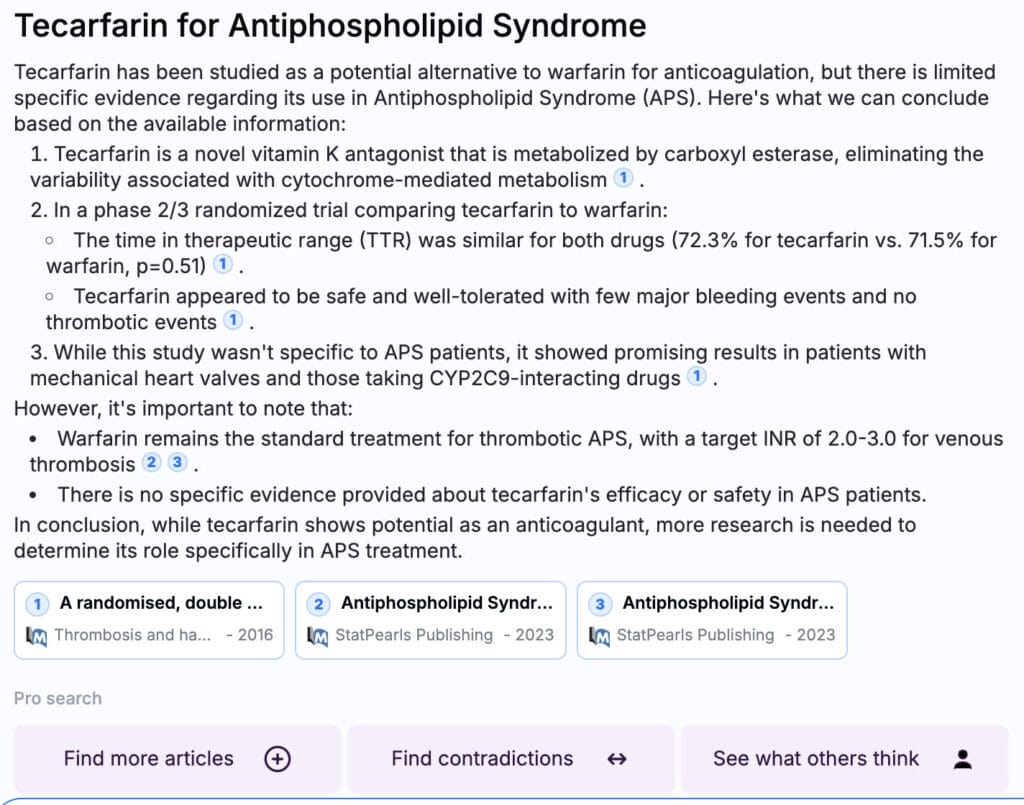
Who is MediSearch for?
MediSearch isn’t only for medical writers, clinicians, or chronic illness patients who have lived with their diagnoses for years. It is also suitable for ‘everyday’ health questions that the average person may have, such as, “is coffee good for health?”, “best foods for reducing cholesterol”, or even “is breakdancing considered a sport?”. Yes sorry, I just had to ask MediSearch about breakdancing, given the Olympics fiasco 😉
Even for ‘simple’ questions such as these, MediSearch cites its sources. I tried asking ChatGPT 4.0 the same question about coffee, and whilst it provided the potentials and drawbacks, no sources were cited. We are living in an age of information overload, disinformation and misinformation, so it’s even more vital to know where the answers generated come from – which MediSearch does.
Every single source it cites is clickable, and taken from actual medical journals, international health guidelines, published books and other credible sources. Regular AI chatbots on the other hand, are fairly limited when it comes to medical questions, as they are only able to retrieve information from open-access or free/public resources.
P.s. To see what the answer is to: “is breakdancing considered a sport?”, simply type the question into the search box on MediSearch’s website. 🙂
Benefits of MediSearch Pro Version
Increased Number of Sources to Refine Accuracy Further
The answers you have seen in this review thus far are all from the MediSearch Pro version. Whilst the standard version gives concise answers as well, the MediSearch Pro version sources from more medical articles, which further refines accuracy.
A sample from the standard version can be seen from the screenshot below. If you compare this to the other screenshots we have seen thus far, whilst it is still evidence-based and informative, the answers from the Pro version are more detailed and streamlined. For the example question below, “is coffee beneficial for health?” – the standard version cites two references, whereas the Pro version gave me 10.
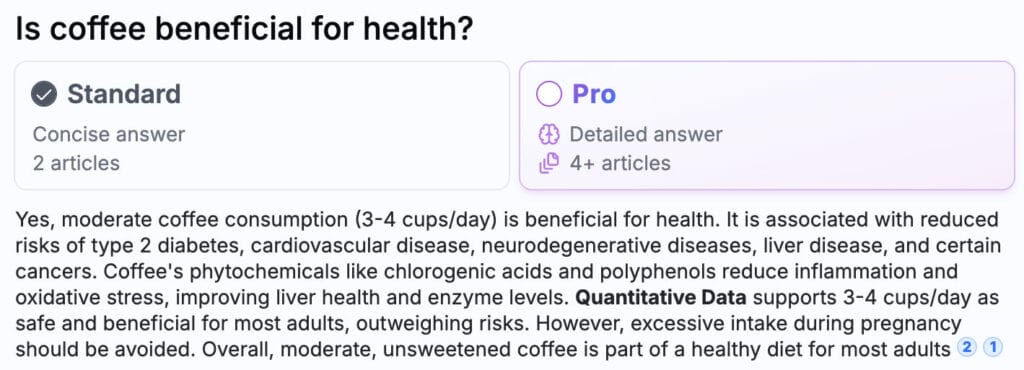
Advanced Filter Options and Citation Tools
If you use Google Scholar, then I’m sure that you’ve clicked on ‘filter by publication date’ at some point, because you want the latest information about a specific topic. MediSearch Pro has a filter by date feature as well, and you can also select which type of sources you want it to search from, such as “scientific articles” and “books”.
If you are a medical writer or need to compile a list of references, MediSearch Pro’s citation tool comes in handy. I personally gather all my references using Zotero, and the ‘export’ feature in MediSearch Pro is compatible with it, including its browser extension. This will save me so much time for research-based articles I write in future.

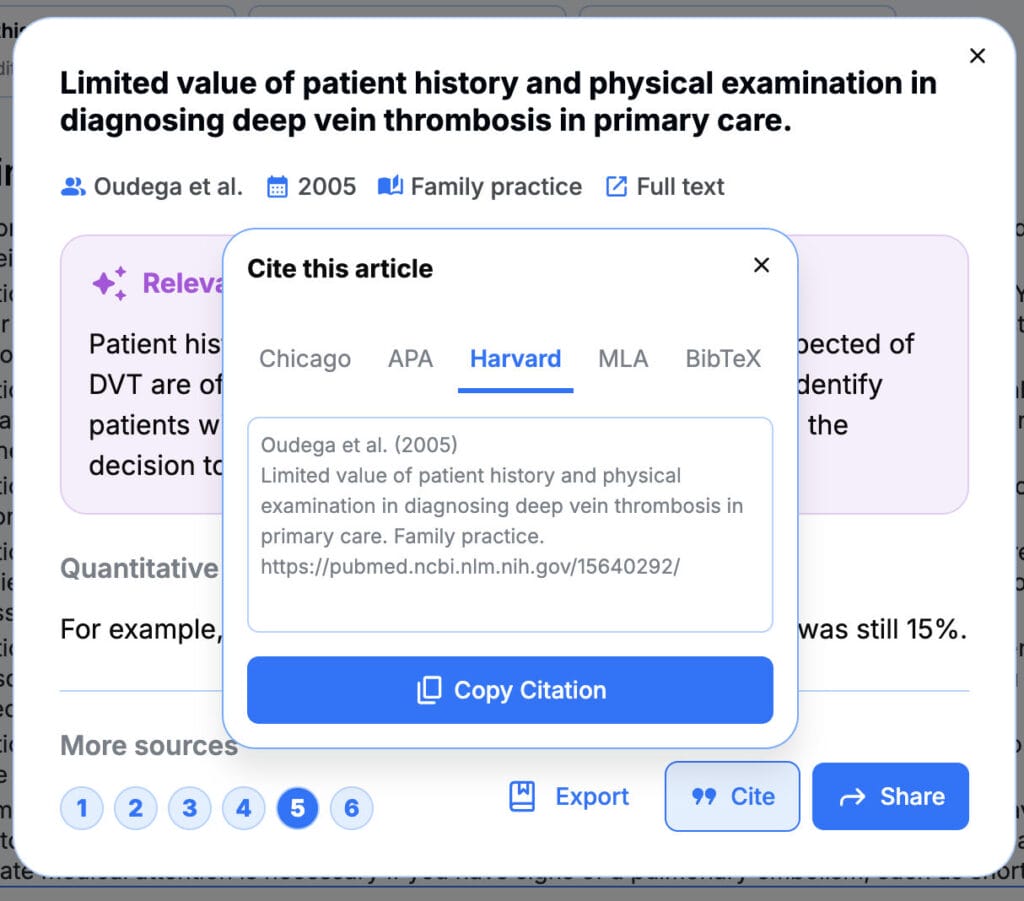
Search for Related Insights with a Click of a Button
In addition, the Pro version also allows you to search for more related articles, find contradictions and see what others think. These additional insights are important if you’re doing research – whether for personal or work related purposes.
If you’ve done research for anything at all (shiny objects included), then you know how important perspectives can be. It is good to have all the cards laid out on the table, so that you can make better judgement calls. The “find contradictions” feature to me is a very good one, because it questions the initial answers to see if there may be potential loopholes.
The “see what others think” feature is also quite interesting, although I personally wouldn’t use it much. It essentially peeks into Reddit threads to see what others have been asking or thinking about in relation to your topic.
This may be a personal preference thing however, as I don’t even trust Reddit on a regular day (I may be a millennial…). I do know that many of my Gen Z friends use Reddit more than even Google Search however, so I can see how this is useful. In their own words, “it gives me human, straightforward answers, and not some lengthy blog with a biased opinion”.
Another thing you could potentially do is to see what others are asking or thinking, rephrase it into a specific question, then feed it back into MediSearch to find out what the science actually says.
Other Video Reviews Available on MediSearch Pro by Health Professionals
If you hate to read and prefer to watch a video to see how best to utilise MediSearch Pro, here are some great reviews by medical professionals and/or establishments:
How to Use MediSearch for Your Medical Writing (by Alex Evans, PharmD, MBA):
Dr. Vimalakar Reddy of KIMS-SUNSHINE Hospitals reviews Medisearch AI tool:
More for the Technically-Inclined and Businesses
MediSearch comes with documentation for developers. You will need an API key to integrate MediSearch into your website or app, which can then be used to generate a medical Q&A chatbot.
Medical businesses or establishments can also use MediSearch to benefit both clinicians and patients. For patients, MediSearch Pro can be used to generate evidence-based health tips, based on individual user data. For clinicians, MediSearch can be used to manipulate Electronic Health Records (EHR) for summaries and also in other novel ways.
Conclusion to My MediSearch Review: Would I Get the Pro Version as a Chronic Illness Blogger and Patient?
The answer is a resounding “yes”. I honestly loved how streamlined, concise and accurate the answers were, and the intuitive user interface. If you have been following my blog for a while, you would know that I recently published an APS A – Z resource guide. This resource took me years to complete, and is truly a work-in-progress. There is still a lot of information that I would like to add to it, such as a related article about herbs, foods and drinks to avoid with APS. With MediSearch Pro, I know that the research process will go much quicker this time around, and I’m actually excited to get started again.
I also work as a medical writer for my own clients, on topics such as digital healthcare, orofacial pain, oral medicine, vitamins and more. I spend a lot of time doing manual research for each article, which can take me days or weeks – more than the actual writing itself. I can see how MediSearch Pro will be an asset to my medical writing jobs in future as well.
In addition to the website version, you can also download MediSearch on the Apple or Google app store – just click on the buttons below:
Visit the MediSearch Website
Download MediSearch on the Apple Store
Download MediSearch on the Google Store
-
Read Related Posts:
- Antiphospholipid Syndrome Diagnosis: The A to Z Guide as a Patient
- Latest Research on Antiphospholipid Syndrome (2024 Edition)
- The Lowdown on Medications and Antiphospholipid Syndrome (Warfarin, Enoxaparin, DOACs, NSAIDs & More)
- Knee Surgery Post-Operative Care: Introduction to the Series
- Why I Need to See 10 Different Doctors on a Regular Basis
- Advice That Could, Quite Literally, Kill
If you liked this article, sign up for our mailing list here so you don’t miss out on our latest posts! You will also receive an e-book full of uplifting messages, quotes and illustrations, as a token of appreciation!
Pin to Your Medical Technology & Health App Boards:
A Guide to Complete Body Care for Women
*Note from A Chronic Voice: Dr. Ammar Mahmoud is a renowned OB-GYN who specialises in advanced labiaplasty and vaginoplasty techniques. He has a particular focus on sexual wellness and function. In this post, he highlights fundamental yet important tips and reminders on body care for […]
Chronic voices*Note from A Chronic Voice: Dr. Ammar Mahmoud is a renowned OB-GYN who specialises in advanced labiaplasty and vaginoplasty techniques. He has a particular focus on sexual wellness and function. In this post, he highlights fundamental yet important tips and reminders on body care for women. Don’t forget to take care of yourself – both inside and out!
*Disclaimer: This article is meant for educational purposes and is not a substitute for medical advice. Please consult your own doctor before changing or adding any new treatment protocols. Read our Privacy Policy page for more information. Thank you!
Introduction
From adolescence to motherhood and later stages of life, a woman’s body undergoes remarkable changes. Each phase brings unique challenges, from hormonal and bodily changes during adolescence to the physical and emotional demands of pregnancy and motherhood and, later, the effects of menopause and aging on bone density and energy levels.
Beyond treatment of illnesses, you can also focus on nurturing your mind, body, and spirit at every stage in order to build up a more balance and holistic approach to health and women’s wellness. This post is here to inspire and guide you towards a complete body care routine.
How To Take Care of Your Body
1. Nutrition
A balanced diet forms the foundation for optimal health for women. It’s essential to consume a variety of macronutrients, such as carbohydrates, proteins, and fats, to fuel your body and support its functions. Carbohydrates provide energy, while proteins are crucial for tissue repair and muscle maintenance. Fats from foods like avocados, nuts, and olive oil play a key role in supporting hormonal balance and boosting overall health.
While a balanced diet should ideally supply all your nutrients, certain life stages or dietary restrictions may require supplements. For example, women at risk for osteoporosis might consider calcium and vitamin D to support bone health. As with nutrition, hydration is also essential for overall well-being. Daily water needs vary, but a good sign of adequate hydration is pale and clear urine.
2. Physical Activity and Exercise
Physical activity is essential for women’s wellness, and staying active can lower the risk of mortality and prevent and help manage heart disease, diabetes, and cancer, while also improving brain health and reducing symptoms of depression and anxiety. For pregnant women, physical activity can reduce the likelihood of complications without raising the risk of low birth weight or stillbirth.
Here’s the good news: physical activity covers pretty much anything that gets you moving and burning energy. Whether you’re walking, doing chores, or playing with your kids, it all counts towards better health. For maximum benefits, aim for 150–300 minutes of moderate aerobic exercise or 75–150 minutes of intense activity each week.
Additionally, pelvic floor exercises like Kegel exercise are vital for strengthening the muscles that support the bladder, uterus, and rectum, promoting better core stability and preventing issues such as incontinence.
3. Intimate Health and Wellness
Maintaining intimate hygiene is essential for overall health. Stick to washing the vulva with water and a mild, unscented soap if you want. The vagina cleans itself, so there is no need for extra products; steer clear of harsh soaps, douches, and heavily scented stuff, as they can mess with your natural balance and lead to irritation or infections.
Hormonal changes, especially after childbirth or during menopause, can lead to dryness, discomfort, or changes in how things look and feel down there. For some, these changes can affect confidence and daily comfort. That’s where pelvic floor exercises and vaginal rejuvenation surgery come in, as they can help with issues like muscle tone and laxity! If you’re considering vaginal rejuvenation procedures, consult with a healthcare provider to ensure it’s right for you.
Don’t skip those regular gyno check-ups, either. Pap smears, screenings, and self-exams are essential for catching infections or abnormal growths early.
4. Mental and Emotional Health
Taking care of your body as a woman involves physical health and prioritizing mental and emotional well-being.
Stress management is crucial; techniques like mindfulness, meditation, and breathing exercises can help you stay grounded and reduce anxiety. Engaging in self-care practices is equally important. Activities like journaling, pursuing hobbies, and finding time for relaxation can foster joy and help you recharge. Whether painting, gardening, or reading a book, making time for what you love can significantly boost your mood and resilience.
Finally, it is vital to recognize the importance of mental health resources. Therapy and counseling can provide essential support, especially during challenging times. Be aware of signs that it might be time to seek help, such as persistent feelings of sadness, overwhelming stress, or difficulty coping with daily life.
5. Skin and Hair Care
Your 20s are a great time to start a skincare routine and develop healthy habits for your skin. But if you’re past that age, don’t worry It’s never too late to begin! Your skincare routine should match your skin type, age, and specific concerns. But the essentials are simple: start with a gentle cleanser that works for you, follow up with a moisturizer to hydrate and protect your skin, and don’t forget sunscreen with at least SPF 30 whenever you head outside.
Add some science-backed ingredients if you want to level up your routine and address specific concerns. Retinoids are awesome for tackling fine lines and wrinkles, while vitamin C helps fade dark spots and signs of aging. Ceramides boost your skin barrier, and peptides help your skin produce more collagen.
Knowing your hair type helps you choose products that actually work, whether your hair is curly, straight, exemplary, or thick. Shampoo is based on how frequently your hair gets oily or dirty, focusing on the scalp to avoid drying out the strands. Make sure to follow up with the conditioner every time to detangle and moisturize.
Be gentle, especially with wet hair. Detangle using a wide-tooth comb, starting from the ends and working up, and try wrapping your hair in a towel or t-shirt instead of rubbing it dry. Limit heat styling, and always use a heat protectant if you do.
Key Takeaways and Final Thoughts
A holistic approach to body care is significant because it recognizes the interconnectedness of physical, mental, and emotional health, allowing women to thrive in all areas of life.
Remember, taking care of yourself is essential for living a balanced and fulfilling life. It enables you to navigate challenges with confidence and joy. Embrace this journey of self-care and make it a rewarding part of your everyday routine.
-
Read Related Posts:
- Pregnancy, Miscarriage & Women’s Health in Antiphospholipid Syndrome
- After Surgery Care at Home: Hygiene Resources
- How to Use the 7 Dimensions of Wellness to Thrive with Chronic Pain
If you liked this article, sign up for our mailing list here so you don’t miss out on our latest posts! You will also receive an e-book full of uplifting messages, quotes and illustrations, as a token of appreciation!
Pin to Your Body Care for Women Boards:

Contributor Bio

Essential Gluten-Free, Dairy-Free, and Nut-Free Foods List for Easy Shopping
Adapting to a gluten-free, dairy-free diet can be challenging if you’re unsure of where to start. If you have additional food allergies or food sensitivities, finding foods to eat can seem nearly impossible. This list of gluten-free and dairy free foods will take the mystery […]
mind-&-emotionsAdapting to a gluten-free, dairy-free diet can be challenging if you’re unsure of where to start. If you have additional food allergies or food sensitivities, finding foods to eat can seem nearly impossible. This list of gluten-free and dairy free foods will take the mystery out of shopping. And if you’re avoiding peanuts and tree nuts, you’ll also find what you need here.
This post contains affiliate links. If you make a purchase through a link, I may receive a small commission, at no cost to you.
Often, the symptoms which lead you to choose a gluten-free, dairy-free diet don’t give you the luxury of time to figure things out.
Medical conditions like celiac disease and non-celiac gluten sensitivity often come with a host of unpleasant symptoms. The same is true with allergic reactions, especially to dairy, peanuts, and tree nuts.
Consuming foods with these products can cause life threatening allergic reactions.
This gluten-free guide will help you fill your kitchen with safe and delicious food.
What is gluten
Gluten is a type of protein found in wheat, rye, spelt, barley, and malt. It helps baked goods retain their structure and moisture. Gluten found in wheat flour is what gives bread its elasticity. Without gluten, baked goods can crumble easy.
Gluten also acts as a thickening agent.
Why go gluten-free
Studies have shown improved outcomes when gluten was removed from the diets of susceptible people. This includes people with:
- Celiac Disease
- Non-Celiac Gluten Sensitivity
- Autoimmune Diseases
People with celiac disease (CD) suffer from damage to the small intestines when consuming gluten. This often results in abdominal pain, malabsorption, and nutritional deficiencies. It can even lead to infertility, depression, osteoporosis, and cancer.
People with non-celiac gluten sensitivity (NCGS) can experience abdominal pain, constipation, diarrhea, migraines, allergies and joint pain.
Gluten and inflammation

Gluten has been attributed to the development of leaky gut syndrome. This occurs when the intestinal barrier that keeps food proteins from passing into the bloodstream gets compromised. The resulting inflammation can trigger:
- Inflammation
- Allergies
- Eczema
- Autoimmune disease
What is dairy
Dairy includes all milk and milk products derived from mammals. This includes cows, sheep, goats, and buffalo. Eggs are often mistaken as dairy, but they’re not. Eggs come from birds which are not considered mammals.
Who should avoid dairy products
People with a dairy allergy should not consume dairy products.
People with lactose intolerance lack the enzyme to digest natural sugars found in milk. This can lead to uncomfortable symptoms including gas, bloating, diarrhea, and stomach discomfort. Eliminating milk can halt these uncomfortable symptoms.
The Problem with Food Labeling

The FDA requires manufacturers to identify common allergens on food labels. This includes gluten and wheat. Gluten, unfortunately, did not make the list. Identifying the presence of wheat is only half the battle.
Gluten can be found in other ingredients like rye, barley, malt, and spelt. Those of us who avoid gluten are forced to play the guessing game.
For this reason, your safest bet is to only eat foods with the certified gluten-free label. But that’s only ¾ of the battle. Because unless you know which foods have the gluten-free label, grocery shopping can be long and painful!
I’m going to take away some of that guesswork for you. I’ve been gluten-free since 2017. Through the years I’ve found some tried and true gluten-free products that have become kitchen staples.
Even with this knowledge, I always double-check the label before putting groceries in my cart. Manufacturers are known to change product ingredients without notice.
What can I eat on a gluten-free, dairy-free diet
Whole foods purchased in their natural state can be eaten without any problem. This includes:
- Eggs
- Fresh fruits including apples, oranges, bananas, and melons
- Whole vegetables such as kale, spinach, squash, sweet potatoes, and carrots
- Fresh meat including chicken, beef, pork, and lamb. Avoid processed meats as some can contain gluten.
- Fresh herbs like rosemary, basil, and thyme
- Legumes like peanuts, chickpeas, lentils, black and red beans, peas
- Oils including olive oil, vegetable oil, and coconut oil
The shopping list above is an abbreviated list. Feel free to eat any whole foods purchased in their natural state.
Any food labeled “gluten-free” can be consumed. Below is a list of tried and true gluten-free, dairy free foods, and nut free foods.
Essential List of Gluten, Dairy and Nut-Free Foods to Buy
Years ago, you had to go to stores like Whole Foods or Trader Joe’s to find foods to accommodate a gluten-free diet. These days gluten-free products are widely available at all major grocery stores.
Bread
Canyon Bakehouse Bread Mountain White Bread is the best gluten-free bread in my opinion. It tastes and feels close to regular bread. Your sandwiches won’t fall apart like some other brands I tried, even with tuna fish.
Canyon Bakehouse Bread comes in several varieties including:
Most grocery stores only carry 2 or 3 varieties, so purchasing other vari eties online may be your best bet..
Cupboard Essentials
Flour
Wheat flour contains gluten. You can find a variety of gluten-free flour blends in most large supermarkets. I make my own gluten-free all-purpose flour blend using brown rice flour. I’ll alternate between Arrowhead Mills Brown Rice Flour and Bob’s Red Mill Brown Rice Flour, depending on what’s available at my local grocery store.
I also add:
If you’re making baked goods or pancakes, you’ll want to add some. This acts as a binder, holding the structure together. It also helps baked goods retain moisture and gives them elasticity.
Check out my article, How to Make a Versatile Gluten-Free All-Purpose Flour Blend.
Oatmeal
Even though oatmeal is gluten-free, cross-contamination can happen during the manufacturing process. For this reason, oatmeal sourced from gluten-free oats is the best option. For a fiber rich oatmeal try Bob’s Red Mill Quick Cooking Rolled Oats contains 4 grams of fiber.
You May Also Want to Read
High Fiber Gluten-Free Breakfast Recipes to Start Your Day Right
20 Gluten-Free High Fiber Dinner Recipes
Free Constipation Printable List of High Fiber Foods
How to Make a Versatile Gluten-Free All-Purpose Flour Blend
Soy Sauce
Gluten can be sneaky, hiding out in products like soy sauce. Liquid Aminos is a gluten-free alternative that can be used in place of soy sauce. Sometimes I’ll use Kikkoman Gluten-Free Soy Sauce if Liquid Aminos is unavailable. But Kikkoman has a distinct flavor, and that might not work well for all dishes.
Other Cupboard Essentials
- Bob’s Red Mill Gluten Free Cornmeal
- Carolina Long Grain Rice
- Carolina Brown Rice
- Simpli White Quinoa
- Barilla Gluten-Free Pasta
- Gravy master
- Prego Traditional Sauce
- Kirkland Pure Maple Syrup
- Pacific Foods Chicken Broth
Snacks
- Enjoy Life Chocolate Chips Baking Morsels
- Nature’s Bakery Gluten Free Fig Bar
- Skinny Pop Popcorn (plain)
- Late July Organic Restaurant Style Tortilla Chips
Fridge and Freezer Essentials

Milk
These days there’s no short supply of dairy-free alternatives for cow’s milk. While cashew, macadamia, and almond milk are sourced from nuts, other options exist. Soy milk and oat milk are 2 popular dairy alternatives. Not all of these are gluten-free so be sure to read the labels. Rice milk is also widely used. I use Dream Organic Rice Milk in place of milk for all my recipes.
Ice Cream
Like milk, gluten-free ice cream is more often than not made with nuts. So Delicious Cookies and Cream ice cream is sourced from coconut milk.
Yogurt
So Delicious Dairy-Free yogurt is sourced from coconut milk. It has a thick, creamy texture similar to Greek yogurt. Silk yogurt is a soy-based yogurt. Both are available in an assortment of flavors.
Tips for Gluten-Free Shopping
Since manufacturers are not required to identify gluten content in their products, care should be taken.
- Always Read Labels: Even if a product seems naturally gluten-free, it’s important to check the label for hidden gluten or potential cross-contamination.
- Look for Certification: Products labeled with a gluten-free certification have been tested and are considered safe for those with gluten sensitivities or celiac disease.
- Watch Out for Cross-Contamination: Some products may be processed in facilities that also handle wheat, so opt for items specifically labeled gluten-free to avoid contamination.
- Always read the label for rice blends as they contain spices and other ingredients that may contain gluten.
Conclusion
By stocking up on these gluten-free essentials for your fridge and cupboards, you’ll have a wide variety of ingredients on hand to create delicious, safe, and satisfying meals. Whether you’re cooking from scratch or looking for easy meal options, this list of gluten and dairy-free Foods will help you maintain a healthy and gluten-free lifestyle.
The post Essential Gluten-Free, Dairy-Free, and Nut-Free Foods List for Easy Shopping appeared first on Health Uprising Now.

Tell Me You’re Chronically Ill Without Telling Me You’re Chronically Ill (51 Chronic Illness Memes)
Darkness Needs Lightness for Balance… All of my recent posts have been extremely ‘heavy’, so to speak. First, there were the two knee injury series – one on resources for post knee surgery, and the other on things you can do whilst bed bound. Then, […]
Chronic voicesDarkness Needs Lightness for Balance…
All of my recent posts have been extremely ‘heavy’, so to speak. First, there were the two knee injury series – one on resources for post knee surgery, and the other on things you can do whilst bed bound. Then, there was the Antiphospholipid Syndrome A to Z resource, which included a few other topics such as medications, women’s health, the latest APS research and all the major organs in the body that the autoimmune disease can hit.
Researching and writing those articles consumed a lot of my brain power and energy, which comes in limited edition as a person with multiple chronic illnesses. Then, I landed in hospital with more new diagnoses just a few weeks after school re-opened…..
…Or Maybe It Just Needs More Darkness!
So I decided to do this post for a bit of fun, and to take a break from the dreariness of it all. A metaphorical digestif, if you will. This post is part of a TikTok trend (I should really get on it some time soon, shouldn’t I?), “Tell Me Without Telling Me”. I learned about it from a post by Caz over at invisiblyme.com, although I can’t seem to find the original post now. Many of us who live with chronic illness endure our days with chronic pain, chronic fatigue, brain fog and other unnameable unpleasantries.
Humour has always carried me through the darkest periods of chronic illness, especially when faced with mortality. Morbid, dark humour is my favourite. It somehow lightens the whole situation, and makes things seem less scary or foreboding. To be able to laugh into the face of death takes away some of its power, and lightens the load. It gives me the strength to carry on.
What about you? What sort of humour do you enjoy the most, and does it help you through the dark days? Check out these “Tell Me You’re Chronically Ill Without Telling Me You’re Chronically Ill” memes I made, and let me know if you can relate to any of them in the comments below!
-
Read Related Posts:
- Chronic Illness Quotes to Inspire, Motivate, Grieve, Hope & Laugh About
- 12 Visible Evidence of a Body Gone Rogue (Is Invisible Illness Truly Invisible?)
- How to Use the 7 Dimensions of Wellness to Thrive with Chronic Pain
- 7 Reminders For Those Bad Days to Keep You Going
- An Open Letter to Death, and One Simple Plea
-
Changelog:
- 03 February 2025: Three new memes added at the bottom of post.
*Disclaimer: This article is meant for educational purposes, and is based on my personal experiences as a patient. I am not a doctor, and nothing in this article should be substituted for medical advice. Please consult your own doctor before changing or adding any new treatment protocols. This post may also contain affiliate links. It will cost you nothing to click on them. I will get a small referral fee from purchases you make, which helps with the maintenance of this blog. Read our Privacy Policy page for more information. Thank you!
“Tell Me You’re Chronically Ill Without Telling Me You’re Chronically Ill” Memes – Can You Relate?
- Autocorrect keeps ‘correcting’ your medical words to something incorrect. No way you actually meant “antiphospholipid” or “encephalomyelitis”.
- Sometimes you wish you were older, just so people would stop questioning the reality of your illnesses because you’re ‘too young’ to be that sick.
- You drill your travel companions on emergency protocols like an army sergeant, just in case you get a seizure or something cool.
- Superfoods and kale juice can land you in the A&E/ER at best, or kill you at worst.

- Your girlie pouch in the bag contains emergency medication (make that medicationS). Maybe lipstick and mascara – if there’s space.
- You can read a medical article in a minute and actually understand all the jargon.
- Choosing the ‘physician’ rather than ‘consumer’ version of medical articles to read.

- Spontaneity means getting prepared to be spontaneous. Unless of course, it’s a trip to the ER.

- You also have a ‘grab and go’ bag even though you’re not pregnant, for that said spontaneous trip to the A&E.
- Also, you don’t just have a backup plan, but the backup plans.

- When the #1 item on your Christmas wish list is simply – less pain. (A girl/boy can dream?)

- Your hands have a ‘daily quota’, so you use other body parts to compensate. Hey, shoulders are more efficient for opening doors, non?
- Gross isn’t gross – it’s important medical information that needs to be described in great detail to doctors so they can diagnose you properly and relieve you of pain.

- You develop naked body confidence, after needing to undress or spread your legs for the doctor/lab tech/whichever medical professional for the umpteeth time. It’s just a body.

- You need to dismantle your sushi because you can’t open your mouth wide enough to take a bite.

- Cutting up steak also requires careful planning and execution. If in company or if your hands are too painful for the day – abort mission and order a miserly salad like you meant to instead.
- That said, you can knock back a fistful of pills like a pro. They should really have a Major League
EatingPill Popping championship, because you would totally rock that. - You also have a ‘pill swallowing method’ where various parts of your mouth cavity serve as storage and launching devices.
- You have chronically ill internet friends who ‘get you’ more than people in real life. These are people you can discuss body parts, bowel movements and pain with all day without judgement.

- Monitoring your energy levels at events has become second nature, especially after you’ve had to make Titanic drama level exits a couple times.
- A shopping spree consists of pyjamas, compression clothing, ice and heat packs, hot water bottles, and mobility aids.

- Your ‘savings’ amount to a grand total of… $0. Those pesky medical bills really need to ease up their enthusiasm for a bit…

- You want to read that 1000-page book but fret, because you know it’s a trade off with pain in your finger and hand joints. (Thank goodness for Kindles!)
- Essential to do on arriving home from ‘the outside world’ – wiping your phone down with a 70% isopropyl alcohol wipe.

- You glance or glare passive aggressively at anyone who coughs or sneezes on the street (or the elevator…gross).
- You’re grateful that the pandemic normalised mask-wearing (speaking for Asia, at least).
- The chemist is like the adult version of a candy store where you restock your OTC supplies.

- When you know the actual medication name – not just the brand name – better than the pharmacist or doctor. No, it’s not just Clexane or Lovenox, it’s enoxaparin to be precise.
- You run a mini pharmacy at home that takes up at least a few shelves. People come to you for medical supplies for minor ailments, or to ask you what their symptoms could be indicative of.

- That mini pharmacy extends to your bedside table, where you keep emergency supplies for immediate access.
- When the GP panics just as much as you, and just directs you to the nearest ER.

- You have a weighted blanket to help manage your anxiety… except you regret buying it because it’s basically a giant paperweight when your swollen hands can’t pull it up at night.
- You hold your bladder in and calculate your toilet breaks like an arithmetic problem, in order to save your knees some pain per trip.

- You also need 5 minutes to mentally prepare yourself just to sit up, when you need to use the toilet at night.
- You can prattle off tongue-twister medical conditions and medications off the tip of your tongue like poetry.

- Your bottle of concentrated peppermint essential oil has saved a drunk friend or two from puking.
- You have two homes. The second being the hospital. Even the staff know you by name.

- The fear of boarding public transportation is real. Often you avoid the disabled seat even if no one is sitting in it, for fear of being accused.
- Same goes for disabled toilets. When you’re actually out with your walking stick or mobility aid, you feel vindicated just standing outside. Look at my mobility aid, goddamnit.
- Home is where the… medications are.

- Your calendar is fully booked for the rest of the year with doctor appointments. Maybe you can squeeze a friend in somewhere, but probably not.
- Your handwriting is like a 4 year-old’s scrawl because your hand trembles, either from illness or a medication side effect.

- When you rupture your tendons, but assume it’s ‘just a dislocation’ that your hypermobile friends online can teach you how to pop back.
- People think you’re cold and arrogant, no thanks to your resting pain face.

- Your idea of a fun, wild night out with friends is chilling on the couch at home, playing board games. Maybe one glass of wine tops, and with a wine wand.
- You’re absolutely shocked when/if you wake up to a pain free day. You poke and prod your body all day in disbelief, and wonder if that’s how ‘normal’ people feel every day?!

- You now consider work stress as a luxury problem, and dream of being stressed out about work, instead of rotting in bed all day long with pain and fatigue.

- You understand that ‘just be happy’ is a bullshit platitude and attitude on life, when you live in chronic pain. So you seek a life with meaning instead.

- When someone asks if you’ve heard of a disease… You can guess based on its medical name.

- You carry a water bottle wherever you go (with at least one sip left) just in case you need to pop that emergency med.

- You know you have a rare disease when… you search a hashtag on social media, and the ‘latest’ post is yours from 2 years ago.


Conclusion to the “Tell Me You’re Chronically Ill Without Telling Me You’re Chronically Ill” Meme Series
Could you relate to any of these memes as a person with chronic illness or disabilities? I’d love to hear which you could relate to the most in the comments below! And if you have a good chronic illness meme of your own, I’d love to hear it too, and perhaps add it to this post (with credits to you, of course)!
Wishing you a low-pain day, and one filled with laughter 🙂
-
Read Related Posts:
- Call Me Sick Girl (Or How to Make Your Weakness Your Strength)
- 365 Mindfulness Journaling Prompts for Self-Improvement
- Today is Not a Good Day to Make Decisions (and That’s Okay)
- Would You Rather: Have an Invisible Illness or a Visible Disability?
- “It’s in My Blood”: Featuring People with Illnesses, Passions & Talents
If you liked this article, sign up for our mailing list so you don’t miss out on our latest posts! You will also receive an e-book full of uplifting messages, quotes and illustrations, as a token of appreciation!
Pin to Your Chronic Illness Memes & Spoonie Humour Boards:

Quick and Easy Ninja Foodi Collard Greens With Bacon Recipe
Do you love the taste of Southern collard greens, but lack the time it takes to make them? Then this quick Ninja Foodi Collard Greens with Bacon recipe is for you! This article will provide step by step instructions on how to whip up a […]
mind-&-emotionsDo you love the taste of Southern collard greens, but lack the time it takes to make them? Then this quick Ninja Foodi Collard Greens with Bacon recipe is for you! This article will provide step by step instructions on how to whip up a batch of southern style collard greens with bacon in less than half the time. [Gluten-Free, Dairy-Free, Paleo, Whole30]
This post contains affiliate links. If you make a purchase through a link, I may receive a small commission, at no cost to you.

Now if you’re a visual person and prefer to see a demonstration, I’ve created a step-by-step video tutorial that shows exactly how I make these Southern collard greens. From soaking and cutting to cooking, every step is covered in an easy-to-follow format.
Feel free to check it out, or continue reading on for the delicious details.
Health benefits of collard greens
I know I don’t need to tell you how delicious Southern Collard greens with bacon are. But did you know that collards have many health benefits? Collard greens are high in Vitamin K which makes them good for maintaining strong bones. Vitamin K also helps blood to clot and encourages healing.
Collards are also a good source of soluble fiber and are rich in antioxidants. Not to mention, collards contain several other nutrients including Vitamins A, C, folate, magnesium, potassium, and phosphorus. In addition to supporting liver health, collard greens can help improve digestive health and reduce inflammation.
Ninja Foodi
Healthy Collard Greens Recipe

For this Ninja Foodi Collard Greens with Bacon recipe, turkey bacon is used. This is lower in fat and sodium than pork bacon, which is high in saturated fat.
The rendered oil is typically used as seasoning in Southern collard greens. Since turkey bacon renders less oil than pork, the turkey bacon is fried in olive oil, a heart healthy fat.
This dish is also made with organic collard greens. Conventional collard greens are sadly on the dirty dozen list. The list is composed by the Environmental Working Group and contains fruits and vegetables with the most pesticides. These pesticides can be toxic.
How do you clean collard greens with salt
Collard greens grow close to the ground. When they’re harvested, they can contain dirt, grit, and even tiny insects. That’s why it’s so important to clean them well. There’s nothing worse than eating a delicious plate of greens only to bite into a mind shattering piece of grit.
Soaking collards in salt water helps to loosen debris and insects. Call me a clean freak, but I like to rinse each individual leaf first to remove visible debris.
Some people like to soak their collard greens whole. I prefer to cut my collard greens before soaking. This allows the salt mixture to reach more surface area. It also makes handling more manageable.
To soak, fill a deep pot with water. Add 1 to 2 tablespoons of salt for each gallon of water. Soak cut greens for 10-15 minutes. Soaking too long can cause collards to lose some of their nutritional value.
Before rinsing, gently agitate greens using your hand. This will further loosen any clinging debris. Drain completely then rinse thoroughly for 3 minutes under running water.
What is the best way to cut collard greens
Before cooking your collard greens, you’ll want to remove the thick, fibrous stems from the base of each leaf. Some people remove the spine as well which is the central stem that runs down the center of each leaf. These spines are thick and take longer to cook.
However the benefit of cooking collard greens in the Ninja Foodi is that leaves are tenderized in only 10 minutes, spines and all! This alleviates the need for having to remove spines prior to cutting.
To cut collards, stack several leaves and tightly roll into a cigar shape. Cut crosswise into 1-inch thick slices using a sharp knife. Repeat until all greens are cut.
You May Also Want To Read
20 Best Pumpkin Dessert Recipes to Indulge in This Fall
30+ Amazing Gluten-Free Soup Recipes to Warm Up Your Fall and Winter

Why do you put vinegar in collard greens
As collard greens mature, their leaves grow larger, tougher and more bitter. The acidity in the vinegar helps to offset the bitterness of the collards. In addition, vinegar helps to tenderize collard greens.
How long does it take greens to get tender
Traditional collard greens cooked on the stovetop can take over 2 hours to cook. Cooking collard greens in the Ninja Foodi cuts this time dramatically! Collards literally cook for only 10 minutes!

Want to see this recipe in action? Watch my full YouTube tutorial for Southern collard greens here: Quick Southern Collard Greens with Bacon.

Easy Ninja Foodi Collard Greens With Bacon Recipe
Equipment
-
1 Ninja Foodi
Ingredients
- 3 bunches Collard greens
- 12 ounces Turkey bacon Cut into 1/2 inch strips
- 1 Onion
- 3 tbsp Olive Oil Extra Light Virgin Oil for Frying and Baking
- 2 cups Chicken Broth
- 1 tbsp Onion Powder
- 1 tbsp Garlic Powder
- 1 tbsp Smoked Paprika
- 1/2 tbsp White Vinegar
- Salt to taste
Instructions
-
Heat olive oil in a skillet and fry the bacon and onions until brown. Start with 2 tablespoons of olive oil and add more if needed. Ideally, there should be 2-3 tablespoons of oil remaining upon completion to be used in the next step.
-
Add bacon and onion mix to cleaned, cut collard greens. Pour remaining oil over the collards.
-
Add garlic powder, onion powder, smoked paprika, and salt to taste. Toss until the greens are seasoned throughout and the oil is evenly distributed.
-
Pour 2 cups of chicken broth into the Ninja Foodi. Add vinegar.
-
Transfer the chopped greens to the Ninja food, and carefully mix with liquid.
-
Set the Ninja Foodi to the pressure cooker setting. Cook on high for 10 minutes, performing a quick release when done to release the steam.
-
Stir the greens to evenly distribute the flavors before transferring to a serving platter.
The post Quick and Easy Ninja Foodi Collard Greens With Bacon Recipe appeared first on Health Uprising Now.